Method Article
Production of A SARS-CoV-2 Virus like Particle System to Investigate Viral Life Cycles In Vitro
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
We present an optimized in vitro protocol for producing SARS-CoV-2 virus-like particles that closely mimic the authentic virus. This approach enables the investigation of viral infection, assembly, and egress mechanisms without the constraints of requiring a biosafety level 3 laboratory.
Streszczenie
The severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) virus-like particle (SC2-VLP) method offers a powerful and accessible tool for studying the SARS-CoV-2 life cycle without the need for biosafety level 3 (BSL-3) laboratories. This system effectively mimics critical stages of the viral life cycle, including assembly, genome packaging, and egress, using a luciferase reporter fused to the T20 signal for sensitive and precise detection of viral particle production. SC2-VLPs are generated by co-expressing SARS-CoV-2 structural proteins, including membrane (M), nucleocapsid (N), envelop (E), and spike (S), along with the RNA packaging signal in HEK-293T cells. Unlike traditional virus-like particle systems, the SC2-VLP method ensures accurate quantification and greater fidelity to the natural viral life cycle. Furthermore, compared to lentiviral pseudotyping methods, which are limited to studying viral entry through the incorporation of S protein into HIV-based lentiviral particles, the SC2-VLP system provides a more comprehensive platform for exploring multiple stages of SARS-CoV-2 biology. While this method bypasses the risks of handling live virus and expands accessibility. The SC2-VLP method represents a significant advancement in antiviral research and the development of therapeutic strategies against SARS-CoV-2.
Wprowadzenie
The COVID-19 pandemic has emerged as one of the most devastating global health crises in modern history, resulting in millions of deaths worldwide1. The virus responsible, SARS-CoV-2, follows a complex life cycle that includes key stages such as infection, genome replication, assembly, and egress. The infection process begins when the viral spike protein (S) binds to the host cell receptor, Angiotensin-Converting Enzyme 2 (ACE2), facilitating the release of the viral genome into the host cell2,3. The viral RNA-dependent RNA polymerase (RdRp) then catalyzes the replication of the genomic RNA. This RNA, in complex with the nucleocapsid protein (N), forms a stable structure that is recognized by the membrane protein (M). The M protein plays a central role in viral assembly by recruiting the RNA-N complex, S, and the envelope protein (E)4,5. After assembly, the virion completes its egress through a noncanonical lysosome-mediated trafficking pathway6.
In response to the pandemic, substantial global resources have been mobilized to develop vaccines, neutralizing antibodies, and antiviral drugs. The evaluation of these interventions has been essential in advancing SARS-CoV-2 research7. However, studying the live virus presents significant logistical challenges, as experiments involving the virus must be conducted in Biosafety Level 3 (BSL-3) laboratories. The limited availability of BSL-3 facilities has constrained the pace of research aimed at understanding and combating SARS-CoV-2.
To address these challenges, two major systems-virus-like particle (VLP) and lentiviral pseudotyping-have been widely adopted in SARS-CoV-2 research, both of which do not require BSL-3 containment8. The VLP system involves the co-transfection of cells with genes encoding viral structural proteins, including M, S, E, and N, which together generate virus-like particles. These particles mimic the structural and functional properties of the virus, making them a valuable tool for studying key processes in the SARS-CoV-2 life cycle, and even an effective antigen for vaccine development9,10,11.
Conversely, the lentiviral pseudotyping system involves replacing the Vesicular Stomatitis Virus (VSV) G protein in lentivirus with SARS-CoV-2 S protein, enabling the production of lentiviral particles that can incorporate reporter genes such as luciferase or GFP. This system is particularly useful for investigating neutralizing antibodies that block the S-ACE2 interaction12. However, lentiviral pseudotyping does not mirror SARS-CoV-2 viral assembly or egress due to the use of HIV structural proteins, which mediate particle release at the plasma membrane.
To overcome these limitations, Syed et al. recently identified the SARS-CoV-2 packaging signal within its RNA genome, which demonstrates the N protein's specificity toward viral genome recognition13. By fusing this packaging signal to reporter genes, it is possible to efficiently incorporate these genes into SARS-CoV-2 virus-like particles (SC2-VLPs)13. This strategy not only replicates the SARS-CoV-2 assembly and egress processes but also allows for the sensitive measurement of infection steps. In this study, we introduce the experimental methodology for using the SC2-VLP system and highlight key considerations for conducting this approach.
Protokół
1. Generation of SC2-VLPs
- Seed ~3.0 × 106 HEK-293T cells in a 10 cm diameter tissue culture plate with DMEM complete medium, supplemented with 10% v/v FBS and 1% penicillin-streptomycin.
NOTE: To ensure high transfection efficiency and optimal SC2-VLP production, HEK-293T cells should be maintained at low passage numbers ~10. - Culture the HEK-293T cell at 37 °C, 5% CO2 for about 24 h, and check the cell confluency under the microscope. Proceed if ~70% confluent.
- Dilute 60 µL of PEI from 1 mg/mL stock to 200 µL with serum-freemedium.
- Add 6.7 µg of N plasmid, 10 µg of Luc-T20 plasmid, 0.016 µg of S plasmid, and 3.3 µg of M-IRES-E plasmid into 200 µL of serum-free medium (see Supplemental File 1).
- Gently add the diluted PEI from step 1.3 into the solution containing plasmids coding for viral structure proteins from step 1.4, and incubate at room temperature for 10 min. This is the transfection solution.
- Carefully drop the transfection solution from step 1.5 onto HEK-293T cells, and gently swirl the tissue culture plate for thorough mixing.
- Exchange the cell culture medium 6 h post infection with the DMEM complete medium, and incubate the transfected HEK-293T cells at 37 °C, 5% CO2 for 48 h.
- Collect the supernatant of the infected HEK-293T cells, which contains the SC2-VLPs, and then filter the supernatant through a 0.45 µm syringe filter to remove cell debris. This is the SC2-VLP medium.
NOTE: We attempted to produce SC2-VLPs in HeLa, Vero E6, and Caco2 cell lines, but no measurable viral titer was obtained, indicating the protocol's specificity for HEK-293T cells.
2. Examination of SC2-VLP effectiveness
NOTE: The HEK-293T cell line stably expressing ACE2 and TMPRSS2 was established using a lentiviral transduction approach14,15. Protein expression of both ACE2 and TMPRSS2 was confirmed by western blot analysis, following a protocol similar to that described in Step 3 (SC2-VLP composition analysis).
- Seed 4.0 × 104 HEK-293T cells with stable expression of ACE2 and TMPRSS2 in a 96-well plate and add 50 µL of SC2-VLP medium from step 1.8.
- Incubate the 96-well tissue culture plate at 37 °C with 5% CO2 for 24 h.
- Remove the medium from the 96-well plate, and wash once with 100 µL of PBS buffer at 37 °C, containing 137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, and 1.8 mM KH2PO4.
- Lyse the HEK-293T ACE2/TMPRSS2 cells with 20 µL of passive lysis buffer, gently rocking the sample for 15 min on an orbital shaker at room temperature.
NOTE: The lysis buffer contains 25 mM Tris-phosphate (pH 7.8), 2 mM DTT, 2 mM 1,2-diaminocyclohexane-N,N,N′,N′-tetraacetic acid, 1.25 mg/mL lysozyme, 2.5 mg/mL BSA, 10% glycerol, and 1% Triton X-100). - Spin the 96-well plate at 4,000 × g for 15 min at 4 °C in a refrigerated microplate centrifuge, and then immediately transfer the plate to an ice bath.
- Take 100 µL of reconstituted luciferase assay buffer to an opaque white 96-well plate, and add 20 µL of lysate from step 2.5. Mix them briefly by pipetting up and down 2-3x.
- Measure the luminescence using a plate reader with the following parameters: Detection mode: Luminescence; Wavelength range: Full spectrum; Plate format: 96-well standard opaque plate; Integration time: 200 ms.
3. Examination of the SC2-VLP composition
- Add 1.36 mL of PEG 8000 solution, containing 50% PEG 8000 and 2.2% NaCl, to 10 mL of SC2-VLP medium from step 1.8.
- Keep the mixture on an orbital shaker, and slowly mix the solution at 4 °C overnight.
- Centrifuge the solution at 4 °C, 2,000 × g for 30 min, and collect the SC2-VLP pellet for western blotting analysis16.
NOTE: For the western blotting analysis, all information regarding the antibodies is provided in the Table of Materials.
4. Subcellular localization analysis of S and its mutants in SC2-VLP-producing cells
- Seed ~3.0 × 106 HEK-293T cells evenly in the glass-bottom culture dish with 15 mm diameter, and then allow the cells to adhere and grow until ~70% confluency before transfection.
- Repeat the transfection procedure as described in steps 1.3 through 1.7 and modify only the plasmid quantities as follows: N plasmid: 1.3 µg, Luc-T20 plasmid: 2 µg, S plasmid: 0.0032 µg, and M-IRES-E plasmid: 0.66 µg.
- Gently wash the culture dish twice with 1 mL of ice-cold PBS, and then add 1 mL of 4% paraformaldehyde (PFA) fixation solution at room temperature (RT) for 15 min.
- Wash the cells for 2 x 5 min with 1 mL of PBS at RT, and then permeabilize the cells by adding 1 mL of 0.25% Triton X-100 at RT for 10 min.
- Wash the cells for 2 x 5 min with 1 mL of PBS at RT, and then add 1 mL of 5% bovine serum albumin (BSA) at RT for 1 h to block nonspecific antibody interactions.
- Add ~200 µL of primary antibody solution (enough to cover the glass bottom) and incubate at 4 °C overnight.
NOTE: The primary antibody solutions are prepared by diluting in 5% BSA dissolved in PBS at the following dilution ratios: the mouse anti-S antibody at 1:200, the rabbit anti-Sec61β antibody at 1:200, the rabbit anti-GM130 antibody at 1:200, and the rabbit anti-ERGIC53 antibody at 1:200. The 5% BSA/PBS solution served as both the diluent and blocking buffer to minimize nonspecific binding during subsequent immunofluorescence staining procedures. - Remove the primary antibody solution, and then wash the cells for 3 x 5 min with 1 mL of PBS at RT.
- Add fluorescence-conjugated secondary antibody solution at RT for 1 h, and then wash the cells for 3 x 5 min with 1 mL of PBS at RT.
NOTE All subsequent steps must be performed in the dark or under minimal light exposure to prevent photobleaching of fluorescent conjugates and preserve signal integrity. Two types of fluorescence-conjugated secondary antibodies, which are derived from mouse or rabbit, are employed to stain either the S protein or cell organelle marker proteins. - Stain nuclei with 2.5 µg/mL Hoechst solution at RT for 5 min, and then wash the cells for 3 x 5 min with 1 mL of PBS at RT.
- Observe S protein or organelle staining and acquire images using a confocal microscope with the following parameters: PMT mode set to VBF (no averaging, line sequential scan) with auto-confocal aperture. For channel 1 (FITC), use the 488 nm laser at 25% power with 500 - 548 nm emission, HV 525 V, gain 1x, and offset 5%. For channel 2 (Alexa Fluor 594), use the 594 nm laser at 25% power with 610 - 670 nm emission, HV 500 V, gain 1x, and offset 5%. For channel 3 (DAPI), use the 405 nm laser at 25% power with 430 - 470 nm emission, HV 490 V, gain 1x, and offset 5%.
Wyniki
The egress and assembly steps of the SARS-CoV-2 life cycle have been less studied than the infection and replication steps17,18. Before the SC2-VLP method was developed, these processes could only be investigated using live SARS-CoV-2, confining research to BSL-3 laboratories13. The SC2-VLP workflow, shown in Figure 1, outlines the experimental protocol and illustrates the processes involved in these steps of the SARS-CoV-2 life cycle. In this approach, plasmids encoding the structural proteins of SARS-CoV-2 (M, E, S, and N) and the RNA packaging signal (T20) are co-transfected into HEK-293T cells. A luciferase reporter fused to the T20 signal enables sensitive detection of the released SC2-VLPs, which can then infect recipient cells expressing the SARS-CoV-2 receptors ACE2 and TMPRSS2, as depicted in Figure 1.
To optimize the amount of plasmid encoding SARS-CoV-2 structural proteins and the packaging signal, particularly the S plasmid, we transfected HEK-293T cells with varying concentrations of the S plasmid. The results revealed that an S plasmid-to-other-plasmid ratio of 1:10 provides the optimal conditions for SC2-VLP production (Figure 2). This finding aligns with a previous report by Syed et al. and reasonably explains why, despite being one of the most abundant components in SARS-CoV-2 virions, the expression level of the S protein is relatively lower compared to the M, N, and E proteins.
The SC2-VLP system serves as a powerful model for studying the SARS-CoV-2 assembly process, faithfully recapitulating both viral envelope formation and genome packaging. Current evidence highlights the central role of the M protein in assembly, facilitating the recruitment of other structural proteins, including N, S, and E. Immunostaining of these proteins reveals their localization within subcellular organelles, likely the ERGIC or cis-Golgi complex, the primary sites of SARS-CoV-2 assembly19,20. This underscores the potential of the SC2-VLP system as a valuable tool for dissecting viral assembly mechanisms. To further probe the role of S in assembly, we introduced the H1271E mutation, which disrupts COPI-mediated S sorting, thereby impairing S incorporation into virions21,22. In recipient cells, this mutation significantly reduced luciferase activity, confirming that the SC2-VLP system not only faithfully recapitulates viral infection but also serves as a powerful tool for investigating SARS-CoV-2 assembly-a process inaccessible to conventional lentiviral pseudotyping systems (Figure 3). We further employed a comprehensive mutational scanning approach, targeting individual residues (1,255-1,273) in the S C-terminal tail to identify additional mutations that, like H1271E, might attenuate virion assembly and reduce viral titers. Figure 3 demonstrates that the E1262H mutation significantly diminishes SC2-VLP production, while the H1271E/E1262H double mutant abolishes it entirely. These results implicate E1262 in potential interactions with unidentified host factors. Further characterization of host proteins binding to this region, particularly those dependent on E1261, may reveal novel mechanisms governing SARS-CoV-2 assembly. Collectively, these findings establish SC2-VLPs as a versatile and physiologically relevant platform for studying viral assembly in cell culture systems.
To assess the subcellular localization of S protein in SC2-VLP-producing cells, we performed immunostaining analysis of both the wild-type S protein and its H1271E mutant. The results demonstrate that the S protein predominantly colocalizes with the cis-Golgi marker GM130, while showing minimal overlap with the ER marker Sec61β or the ERGIC marker ERGIC-53. These findings align with previous observations of S subcellular localization in authentic SARS-CoV-2 infection23. In contrast, the H1271E mutant displayed a diffuse distribution pattern and showed no colocalization with the cis-Golgi marker GM130. This suggests that the mutation disrupts proper localization to the viral assembly site, potentially explaining its impaired ability to facilitate SARS-CoV-2 virion assembly (Figure 4). These results further establish SC2-VLPs as a valuable tool for studying the biological functions of S and other viral structural proteins.

Figure 1: Schematic representation of SC2-VLP production and its applications. The SARS-CoV-2 genomic RNA packaging signal, T20, is highlighted in cyan, while the S protein is shown in dark green. Plasmids encode structural proteins of SARS-CoV-2, including M, E, N, and S, with M and E co-expressed from a single vector. Key stages of the viral life cycle are illustrated, including assembly (light green), egress (light blue), and infection (orange), as indicated by arrows. Abbreviations: SARS-CoV-2 = severe acute respiratory syndrome-coronavirus 2; SC2-VLP = SARS-CoV-2-virus-like particle. Please click here to view a larger version of this figure.
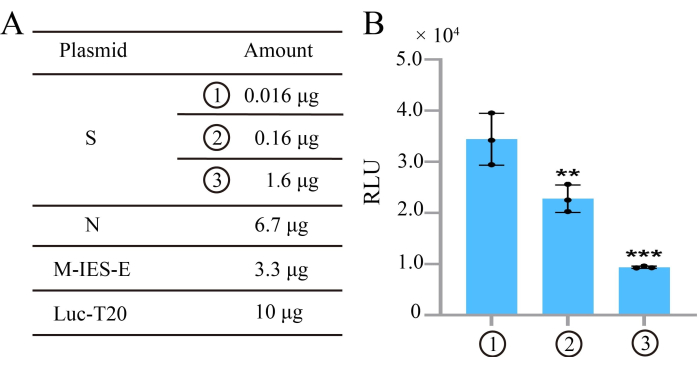
Figure 2: Sensitivity of SC2-VLP titer to the transfected amount of the plasmid encoding S. (A) Table showing the transfection amounts of plasmids encoding SARS-CoV-2 structural proteins and the gRNA packaging signal. (B) SC2-VLP titer varies in response to the transfected amount of the plasmid encoding S. Abbreviations: SARS-CoV-2 = severe acute respiratory syndrome-coronavirus 2; SC2-VLP = SARS-CoV-2-virus-like particle; gRNA= guide RNA; RLU = relative luminescence units. Please click here to view a larger version of this figure.

Figure 3: SC2-VLP system used to investigate S assembly into virions. (A) S mutants affecting COPI trafficking lead to a reduction in SC2-VLP titer. (B) Western blot analysis of SARS-CoV-2 S and N protein abundance in SC2-VLPs. (C) S packaging efficiency calculated from (B), with SC2-VLP abundance normalized to N protein levels. (D) Quantification of SC2-VLP abundance from (B). Abbreviations: SARS-CoV-2 = severe acute respiratory syndrome-coronavirus 2; SC2-VLP = SARS-CoV-2-virus-like particle; RLU = relative luminescence units; Ctr = control; WT = wild type; mut = mutant; NS = non-significant. The band corresponding to the full-length SARS-CoV-2 spike (S) protein is labeled as S, while the S2 fragment (residues 816-1,273) represents the C-terminal portion of the S protein, and a non-specific band between S and S2 is indicated as NS24. Please click here to view a larger version of this figure.
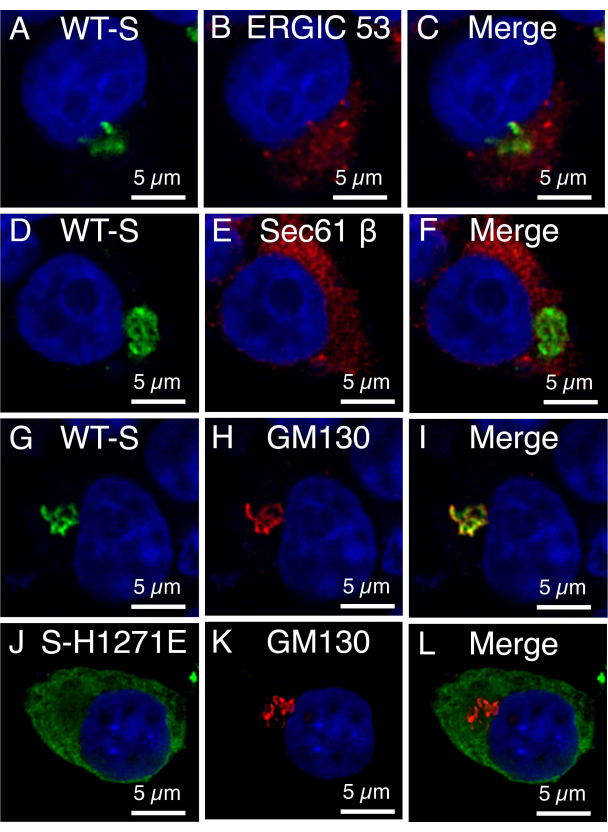
Figure 4: SC2-VLP system used to investigate S subcellular localization. (A-I) Representative immunostaining image of WT S in SC2-VLP-producing HEK-293T cells with co-staining of cell organelle markers. (A-C) ER marker: (D-F) Sec61β, (G-I) ERGIC marker: ERGIC-53; the cis-Golgi complex marker: GM130. (J-L) The colocalization of S E1262H mutant with the cis-Golgi marker GM130. S is shown in green, the cell organelle markers are displayed in red, and the cell nucleus is stained in blue. Please click here to view a larger version of this figure.
Supplemental File 1: DNA sequences of N, Luc-T20 plasmid, S plasmid, and M-IRES-E plasmids. Please click here to download this File.
Dyskusje
A simple and effective method to model the SARS-CoV-2 life cycle in cell culture systems, without the constraints of BSL-3 laboratories, represents a pivotal advancement for anti-SARS-CoV-2 research. The SC2-VLP method fulfills this need, offering a robust and accessible platform. In this study, we provide a detailed protocol for the SC2-VLP method, outlining critical experimental steps for producing SC2-VLPs. Additionally, we highlight its versatility and potential applications in advancing our understanding of SARS-CoV-2 biology and facilitating the development of antiviral strategies.
Traditional SARS-CoV-2 VLP and lentiviral pseudotyping methods are widely used in anti-SARS-CoV-2 research8,25. In the traditional VLP method, SARS-CoV-2 structural proteins M, N, E, and S are co-expressed to generate viral particles26, with their abundance typically monitored by WB analysis. However, viral structural proteins are also incorporated into other membrane structures, such as exosomes, complicating WB analysis of viral particles27. By contrast, the SC2-VLP method incorporates a reporter gene fused to the T20 signal, enabling efficient packaging of the reporter into viral particles. This allows for sensitive and specific detection of particle abundance without relying solely on WB analysis. Furthermore, the SC2-VLP method more faithfully mimics the complete life cycle of live SARS-CoV-2 compared to the traditional VLP method.
The SC2-VLP method surpasses the lentiviral pseudotyping approach in several critical aspects. The lentiviral pseudotyping system relies on the HIV-1 virus framework, in which virions are assembled and budded from the plasma membrane. In contrast, SARS-CoV-2 virions are assembled within the ERGIC or cis-Golgi complex, highlighting a fundamental difference in their life cycles. This discrepancy renders the lentiviral pseudotyping method unsuitable for studying key stages of the SARS-CoV-2 life cycle, such as replication, assembly, and egress, limiting its applicability to the investigation of viral entry and infection.
The SC2-VLP method is a simple and powerful tool for studying the SARS-CoV-2 life cycle. By not involving the authentic virus, this method can be adopted by many laboratories without requiring access to BSL-3 facilities. However, it remains crucial to validate findings derived from the SC2-VLP system using live SARS-CoV-2 to ensure their accuracy and biological relevance.
Ujawnienia
The authors have no conflicts of interest to disclose.
Podziękowania
This work was supported by the Startup fund program at Beijing University of Chinese Medicine (BUCM) (90011451310011). We extend our gratitude to all the member of Dr. Ma lab at BUCM for the invaluable discussion and assistance with the experiments.
Materiały
| Name | Company | Catalog Number | Comments |
| Bovine Serum Albumin (BSA) | Cell Signaling Technology | 9998S | |
| Confocal Laser Scanning Microscope | Olympus | FV3000 | |
| DMEM | Corning | 10-013-CV | |
| Fetal Bovine Serum (FBS) | Thermofisher | A5670402 | |
| Goat Anti-Mouse IgG H&L (Alexa Fluor 488) antibody | Invitrogen | A11001 | dilution ratio: IF 1:1000 |
| Goat Anti-Rabbit IgG H&L (Alexa Fluor 594) antibody | Abcam | ab150080 | dilution ratio: IF 1:1000 |
| HEK-293T cell line | National Infrastructure of Cell Line Resource (NICR) | NICR-293T-001 | To ensure high transfection efficiency and optimal SC2-VLP production, HEK-293T cells should be maintained at low passage numbers (≤ P10). |
| Hoechst 33342 | Invitrogen | H1399 | Working concentration: 2.5 μg/mL |
| Luciferase Reporter Assay System | Promega | E1500 | |
| Luc-T20 | Addgene | 177941 | |
| Mouse monoclonal anti-GAPDH | Proteintech | 60004-1-Ig | dilution ratio: WB 1:20,000 |
| Mouse monoclonal anti-S RBD | Abclonal | A23771 | dilution ratio: IF 1:200 |
| OptiMEM | Thermofisher | 31985070 | serum-free medium for transfection |
| PEG3350 | Sigma-Aldrich | P3635 | |
| PEG8000 | Sigma-Aldrich | P2139 | |
| Penicillin-Streptomycin | Thermofisher | 15140122 | |
| Polyethyleneimine (PEI) | Thermofisher | 43896.01 | |
| Promega passive lysis buffer | Promega | E1941 | |
| Rabbit polyclonal anti-ACE2 | Proteintech | 21115-1-AP | dilution ratio: WB 1:1000 |
| Rabbit polyclonal anti-ERGIC53 | Proteintech | 13364-1-AP | dilution ratio: IF 1:200 |
| Rabbit polyclonal anti-GM130 | Proteintech | 11308-1-AP | dilution ratio: IF 1:200 |
| Rabbit polyclonal anti-S | Abcam | ab272504 | dilution ratio: WB 1:1000 |
| Rabbit polyclonal anti-Sec61β | Proteintech | 15087-1-AP | dilution ratio: IF 1:200 |
| Rabbit polyclonal anti-TMPRSS2 | Abcam | ab109131 | dilution ratio: WB 1:1000 |
| SARS-CoV-2 M-IRES-E plasmid | Addgene | 177938 | |
| SARS-CoV-2 N plasmid | Addgene | 177959 | |
| SARS-CoV-2 Nucleoprotein Rabbit mAb | Abclonal | A21042 | dilution ratio: WB 1:4000 |
| SARS-CoV-2 S plasmid | Addgene | 177960 | |
| Secondary Antibody, HRP, Goat anti-Mouse IgG (H+L) | Invitrogen | 31460 | dilution ratio: WB 1:5000 |
| Secondary Antibody, HRP, Goat anti-Rabbit IgG (H+L) | Invitrogen | 31430 | dilution ratio: WB 1:5000 |
| SpectraMax i3x plate reader | Molecular Devices | SpectraMax i3x |
Odniesienia
- Narayanan, S. A., et al. A comprehensive SARS-CoV-2 and COVID-19 review, Part 2: host extracellular to systemic effects of SARS-CoV-2 infection. Eur J Hum Genet. 32 (1), 10-20 (2024).
- Shang, J., et al. Structural basis of receptor recognition by SARS-CoV-2. Nature. 581 (7807), 221-224 (2020).
- Lan, J., et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 581 (7807), 215-220 (2020).
- Zhang, Z., et al. Structure of SARS-CoV-2 membrane protein essential for virus assembly. Nat Commun. 13 (1), 4399(2022).
- Han, Y., et al. SARS-CoV-2 N protein coordinates viral particle assembly through multiple domains. J Virol. 98 (11), e0103624(2024).
- Ghosh, S., et al. beta-coronaviruses use lysosomes for egress instead of the biosynthetic secretory pathway. Cell. 183 (6), 1520-1535.e14 (2020).
- Andrews, H. S., Herman, J. D., Gandhi, R. T. Treatments for COVID-19. Annu Rev Med. 75, 145-157 (2024).
- Crawford, K. H. D., et al. Protocol and reagents for pseudotyping lentiviral particles with SARS-CoV-2 spike protein for neutralization assays. Viruses. 12 (5), 513(2020).
- Sultana, R., Stahelin, R. V. Strengths and limitations of SARS-CoV-2 virus-like particle systems. Virology. 601, 110285(2025).
- Xu, R., Shi, M., Li, J., Song, P., Li, N. Construction of SARS-CoV-2 virus-like particles by mammalian expression system. Front Bioeng Biotechnol. 8, 862(2020).
- Plescia, C. B., et al. SARS-CoV-2 viral budding and entry can be modeled using BSL-2 level virus-like particles. J Biol Chem. 296, 100103(2021).
- Cruz-Cardenas, J. A., et al. A pseudovirus-based platform to measure neutralizing antibodies in Mexico using SARS-CoV-2 as proof-of-concept. Sci Rep. 12 (1), 17966(2022).
- Syed, A. M., et al. Rapid assessment of SARS-CoV-2-evolved variants using virus-like particles. Science. 374 (6575), 1626-1632 (2021).
- Hoffmann, M., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 181 (2), 271-280 (2020).
- Matsuyama, S., et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc Natl Acad Sci USA. 117 (13), 7001-7003 (2020).
- Alegria-Schaffer, A., Lodge, A., Vattem, K. Performing and optimizing Western blots with an emphasis on chemiluminescent detection. Methods Enzymol. 463, 573-599 (2009).
- V'Kovski, P., Kratzel, A., Steiner, S., Stalder, H., Thiel, V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat Rev Microbiol. 19 (3), 155-170 (2021).
- Yang, H., Rao, Z. Structural biology of SARS-CoV-2 and implications for therapeutic development. Nat Rev Microbiol. 19 (11), 685-700 (2021).
- Katiyar, H., Arduini, A., Li, Y., Liang, C. SARS-CoV-2 assembly: Gaining infectivity and beyond. Viruses. 16 (11), 1648(2024).
- Klein, S., et al. SARS-CoV-2 structure and replication characterized by in situ cryo-electron tomography. Nat Commun. 11 (1), 5885(2020).
- Li, Y., et al. SARS-CoV-2 spike host cell surface exposure promoted by a COPI sorting inhibitor. Acta Pharm Sin B. 13 (7), 3043-3053 (2023).
- Dey, D., et al. A single C-terminal residue controls SARS-CoV-2 spike trafficking and incorporation into VLPs. Nat Commun. 14 (1), 8358(2023).
- Christie, S. M., et al. Single-virus tracking reveals variant SARS-CoV-2 spike proteins induce ACE2-independent membrane interactions. Sci Adv. 8 (49), eabo3977(2022).
- Guo, L., et al. Targetable elements in SARS-CoV-2 S2 subunit for the design of pan-coronavirus fusion inhibitors and vaccines. Signal Transduct Target Ther. 8 (1), 197(2023).
- Mi, D., Hu, J., Qian, Z. A lentiviral pseudotype system to characterize SARS-CoV-2 glycoprotein. Methods Mol Biol. 2610, 187-199 (2023).
- Swann, H., et al. Minimal system for assembly of SARS-CoV-2 virus like particles. Sci Rep. 10 (1), 21877(2020).
- Xia, B., et al. Extracellular vesicles mediate antibody-resistant transmission of SARS-CoV-2. Cell Discov. 9 (1), 2(2023).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone