Research Article
Reinforcement Reconstruction using Fascia Lata Autograft for Rhomboid Paralysis-Induced Scapular Winging
In This Article
Summary
Here, we present a protocol outlining a unique approach to achieving a stable scapulothoracic joint and restoring the dynamics of the rhomboid muscle.
Abstract
Scapular winging caused by paralysis of the rhomboid muscle is a relatively uncommon condition in shoulder outpatient. Despite the paucity, it presents as a debilitating condition with sequelae of poor function and deconditioning. Reinforcement reconstruction and restoring the rhomboid muscle dynamic presents a biomechanical treatment option for patients because of paralyzed rhomboids. Building upon our previous research demonstrating successful myointegration of autologous fascia lata grafts, we introduce an innovative reconstruction surgical technique utilizing these grafts to address rhomboid muscle paralysis. We performed reinforcement reconstruction using fascia lata autograft on a patient for painful scapular winging caused by paralyzed rhomboids and aimed to achieve a normal rhythm of the scapulothoracic joint. The procedure achieved functional restoration and scapular stabilization through reinforcement reconstruction. Postoperative assessment at 6 weeks revealed a full shoulder range of motion, absence of scapulothoracic discomfort, and resolution of scapular winging confirmed by clinical testing. This advancement provides shoulder orthopedic surgeons with a novel biomechanical solution for managing refractory scapular winging.
Introduction
The scapular winging was first described in 17231, and this disease was a rare scapulothoracic disorder characterized by altered motion and positioning of the scapula, known as scapular dyskinesis. This condition manifested as the prominence of the medial border of the scapula relative to the thorax, both at rest and during movement2,3. Abnormal scapular motion arises from the inability of the scapulothoracic muscles to stabilize the scapula against the thorax, and potential causes included neurologic injury, soft tissue and bone abnormalities, or secondary effects from other shoulder joint disorders4. The principal causes of scapular winging are paralysis of the serratus anterior muscle and the trapezius muscle5. Much more rarely, the scapular winging may be due to rhomboid muscle paralysis6.
Traditional treatment measures primarily focused on conservative therapies such as rehabilitation treatments, including ultrasound therapy, transcutaneous electrical stimulation, and shoulder joint kinesitherapy7. However, for patients who do not respond well to these conservative treatments, surgical options like scapulothoracic fusion were eventually required. These surgeries significantly restricted the range of motion of the scapulothoracic joint and were also highly invasive.
Liao et al. found that the fascia lata autograft could fuse with the muscle very well8. Based on that finding, fascia lata could stabilize the scapular if it is fused with rhomboid muscles. Therefore, we performed reinforcement reconstruction using fascia lata autograft for painful scapular winging caused by paralyzed rhomboids and aimed to achieve a normal rhythm of the scapulothoracic joint (Figure 1 and Figure 2).
Protocol
This study was approved by the Ethics Committee of the First Affiliated Hospital of Army Medical University (BIIT2025060)
NOTE: The patient is a 21-year-old male presenting with right scapular pain and a disorder of mobility for over 2 years, during which conservative treatment has proven ineffective (Figure 1A). Preoperative CT scans of the patient's spine and scapula revealed no significant bony abnormalities (Figure 2A).
1. Patient preparation
- Provide standard pre-surgical preparation. Verify the patient's information, surgical site, and allergy history.
2. Surgical preparation
- Administer anesthesia.
- Evaluate the operative risk by assigning a grade based on the American Society of Anesthesiologists (ASA) classification of physical health. The ASA of this case is Grade I.
- Insert at least one large-bore intravenous cannula (14 G or 16 G) into a peripheral vein.
- Monitor the electrocardiogram, arterial pressure (via radial artery cannulation), capnography, pulse oximetry, urinary output, and body temperature.
NOTE: The anesthesiologist manages the intraoperative anesthesia and begins to administer the anesthetic drugs after verifying the patient's information. Both inhalational and intravenous anesthetic techniques were utilized. - Conduct a blood gas analysis to assess blood gas levels and pH during the surgical procedure.
- Insert the absorbable lupine anchor into the vertebral pedicle.
- Position the patient in a prone orientation. Conduct routine disinfection of the surgical area, which included the patient's affected upper limb (including the entire scapula), extending upwards to the neck, downwards to the navel, and laterally to the contralateral scapula.
- Locat the T5 and T10 pedicles under anteroposterior and lateral fluoroscopy using the C-arm. Mark the skin accordingly.
- Make a skin incision approximately 1 cm in length. Bluntly dissect down to the vertebral body using a vascular clamp.
- Place guide devices into the T5 and T10 pedicles. Under C-arm fluoroscopy guidance, carefully insert a suture anchor into the pedicle (Table of Materials, Figure 2B, Figure 3).
- Harvest fascia lata graft (Figure 4).
- Position the patient in a lateral decubitus position (Figure 4A). Beginning at 2 cm from the proximal end of the greater trochanter on the ipsilateral thigh, make a longitudinal incision through the skin and subcutaneous tissue along the lateral aspect of the femur to expose the fascia lata.
- Measure the distance from the medial border of the scapula to the thoracic vertebra (Figure 4B,C) and harvest approximately 18 cm in length and 4 cm in width of fascia lata from the ipsilateral thigh, then remove any residual muscle and adipose tissue from the fascia lata graft (Figure 4F,G).
- Resect the fascia lata graft to two 18 cm 2 cm grafts and fix the ends of the fascia lata grafts with a running whipstitch suture technique with No. 2 high-strength suture (Table of Materials).
- Perform reinforcement reconstruction of the rhomboid major and minor muscles.
- Make a 2 cm incision at the medial border and inferior angle of the scapula, dissect soft tissues, and insert suture anchors (Figure 4D, E).
- Extend one end of the fascia lata graft using a guiding pin to the incisions at T10, then suture and secure the graft using a suture anchor. Subsequently, insert another suture anchor to fix the other end of the fascia lata graft at the inferior angle of the scapula (Figure 4H).
- Perform similar procedures to secure the fascia lata graft at the T5 scapular body and the intersection point between the medial edge of the scapula and the spine of the scapula (Figure 4I).
- After the surgery, discontinue anesthesia and safely stabilize the patient during recovery.
3. Postoperative rehabilitation
- Maintain the affected limb in a neutral position using an abduction orthosis, which provides adequate protection while allowing a controlled active range of motion exercises for the elbow and wrist joints during the initial 6-week postoperative period.
- Instruct the patient to perform shoulder and scapular range of motion exercises after 6 weeks, followed by strength training after 3 months.
- After 3 months, advise the patient to engage in non-competitive shoulder strength sports activities according to their tolerance and gradually return to sports activities.
Results
At 6 weeks postoperatively, the patient had normal shoulder joint mobility, with flexion at 180°, abduction at 180°, internal rotation reaching T7, and external rotation at 75°. There was no pain or discomfort in the scapulothoracic region, and the scapular wing test showed normal results (Figure 1B, Table 1, Table 2).
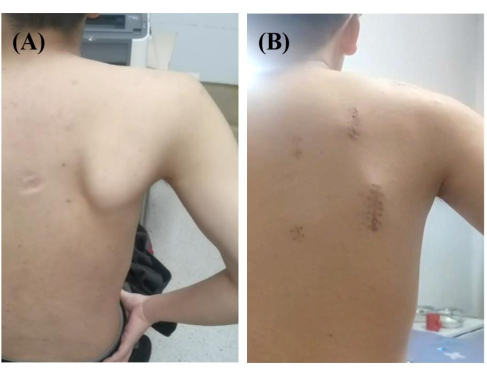
Figure 1: Scapular winging test. (A) Scapular winging test showed a very subtle winging of the scapula, with the scapula laterally translated and the inferior angle rotated laterally. (B) Scapular winging test shows a normal scapular appearance. Please click here to view a larger version of this figure.

Figure 2: Three-dimensional reconstructions. (A) Preoperative and (B) postoperative three-dimensional reconstructions of the right shoulder joint, with the two red circles delineating the insertion points. Please click here to view a larger version of this figure.
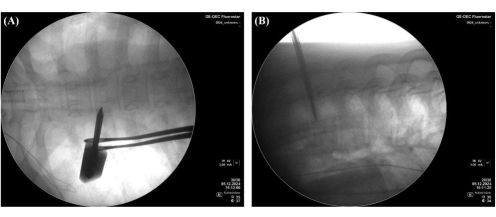
Figure 3: Insertion of the absorbable lupine anchor into the vertebral pedicle under C-arm fluoroscopic guidance. (A) Anteroposterior and (B) lateral radiographic views. Please click here to view a larger version of this figure.

Figure 4: Surgical steps. (A) The incision for inserting the suture anchor into the vertebral pedicles of T5 and T10. (B) Measured the length from the T5 to the intersection point between the medial edge of the scapula and the spine of the scapula. (C) Measured the length from the T10 to the inferior angle of the scapula. (D) Exposed the intersection point between the medial edge of the scapula and the spine of the scapula. (E) Exposed the inferior angle of the scapula. (F,G) Harvested fascia lata grafts. (H) Inserted a suture anchor to the inferior angle of the scapula and extended one end of the fascia lata graft using a guiding pin to the incisions at T10. (I) Extended one end of the fascia lata graft using a guiding pin from the T5 to the intersection point between the medial edge of the scapula and the spine of the scapula. (J) Final view. Please click here to view a larger version of this figure.
| Operative time | 221 min |
| Blood loss | 200 mL |
| Intraoperative fluid infusion | 1500 mL |
| Hospital stay | 6 days |
| Incision healing | Primary healing |
| Other complications | None |
Table 1: Basic surgical information.
| Preoperative | Postoperative | |
| VAS | 3 | 1 |
| Flexion° | 180 | 180 |
| Abduction° | 180 | 180 |
| External Rotation° | 75 | 75 |
| Internal Rotation | T7 | T7 |
| Scapular wing test | Positive | Negative |
Table 2: Preoperative and postoperative functional comparison.
Discussion
Scapular winging was most commonly associated with serratus anterior muscle paralysis, while cases caused by rhomboid muscle paralysis were relatively uncommon. The rhomboid muscle paralysis could lead to winging of the medial border and lateral rotation of the inferior angle of the scapula. Therefore, the surgery technique aimed to restore the stretch of the rhomboid muscle by reconstruction of the paralyzed rhomboid using fascia lata autograft.
Scapular winging was commonly seen in the serratus anterior and trapezius muscle paralysis. In efforts to rectify the scapular winging, various surgical interventions have been employed over the years9,10,11,12. Alfred Tubby first described pectoralis primary transfer for scapular winging in 1904. This surgery technique addressed winged scapula caused by serratus anterior paralysis13. Meanwhile, the scapular winging caused by paralysis of the rhomboid muscle has been linked to myofascial pain syndrome affecting the rhomboids, which may involve entrapment of the dorsal scapular nerve6. The winged scapula caused by rhomboid muscle paralysis was less pronounced on physical examination compared to that caused by trapezius muscle paralysis. Additionally, nerve electromyography reports may not always be accurate, leading to misdiagnosis and potentially resulting in significant disability in the upper limb. Considering that muscle transfer was highly invasive, has a high risk of complications, and changes the rhythm of the scapulothoracic joint, we designed this technique to reinforce the paralyzed rhomboid muscle using fascia lata autograft. In a word, different surgical techniques aimed to restore the normal rhythm of the scapulothoracic joint.
Conservative treatments for winged scapula caused by rhomboid muscle paralysis, including active rehabilitation training, partially alleviated patients' symptoms and remain controversial due to uncertain efficacy. The pectoralis major muscle was transferred from its insertion on the humerus to the inferior angle of the scapular for scapular winging due to serratus anterior muscle paralysis, which stretched the scapular anteriorly14,15. Eden-Lange procedure transferred the levator scapular muscle to the acromion and attached the rhomboid muscles to the central portion of the scapular for scapular winging due to trapezius muscle paralysis16. Modified Eden-Lange procedure transferred the rhomboid minor to the supraspinatus fossa while repositioning the rhomboid major to the infraspinatus fossa. Additionally, the levator scapulae was attached to the spine of the scapula17. Modified Eden-Lange procedure could restore the rhythm of scapulothoracic well. However, the technique involved significant trauma17. Lohre and Elhassan utilized an allogeneic Achilles tendon to connect the scapular spines of the affected and unaffected sides, thereby increasing stability on the affected side18. However, this surgical approach limited the mobility of the unaffected scapula. Scapulothoracic fusion19,20 was considered the last choice for this condition. It might be the best choice to perform reinforcement reconstruction of paralyzed muscle for painful scapular winging caused by different etiology. Reinforcement reconstruction using the fascia Lata autograft technique for paralyzed rhomboid muscle presented a stepwise approach to accomplish the dual goals of stable anatomic reconstruction and restoring the dynamic function, restoring the stretch force of the paralyzed rhomboid muscle. Previous studies have demonstrated that the fascia-muscle interface exhibits favorable healing based on histological findings21,22 Also, Fascia lata was confirmed to reinforce the supraspinatus muscle stretch force through by improving fat infiltration after supraspinatus tendon reconstruction. The lateral termination of the fascia lata grafts was fixed respectively on the footprint of the rhomboid major and minor muscle using the suture anchor. Moreover, the fascia lata grafts were subsequently traversed through the bellies of the rhomboid major and minor muscles, finally fixed on the T5 and T10 vertebral pedicles, respectively. Reinforcement reconstruction was anticipated 6 weeks after surgery to provide an extensive interface healing between the fascia lata graft, trapezius, and rhomboid muscle. Together, the graft can stabilize the scapula and heal at the interface with the trapezius muscle and the rhomboid muscle, thereby restoring the dynamic function of the rhomboid muscle.
The critical steps of this technique included identifying the origin and insertion points of the rhomboid muscle and ensuring accurate insertion of the anchor into the vertebral pedicle. In terms of graft harvesting, the required length of the fascia lata must be measured in advance to ensure surgical precision. Additionally, the use of autologous grafts in this technique effectively avoided the risk of rejection and helped to restore shoulder joint function more quickly. However, this technique was only applicable to scapular winging caused by rhomboid muscle paralysis, with relatively limited indications. It also demanded high diagnostic and surgical skills from the surgeon.
In summary, reinforcement reconstruction of the rhomboid muscle using the fascia lata autograft represents a unique surgical option for the scapular winging caused by rhomboid muscle paralysis. This technique can potentially enhance the rhomboid muscles' static and dynamic functions. High-quality clinical trials using the technique are still necessary for objectively evaluating long-term outcomes.
Disclosures
The authors report no conflicts of interest or financial disclosures related to this work.
Acknowledgements
This research was funded by the Innovation Talents Support Program of PLA’s Ground Force.
Materials
| Name | Company | Catalog Number | Comments |
| Absorbable Lupine anchor | DePuy Mitek | 210712 | For insertion into the vertebral body and scapula, and for fixation of the graft |
| C-shaped X-ray imaging device | General Electric Company | https://www.gehealthcare.com/zh-cn/products/surgical-imaging/oec-one-cfd | The C-arm is utilized for intraoperative pedicle localization and pedicle screw placement |
| Orthocord | DePuy Synthes | https://www.jnjmedtech.com/en-US/product/orthocord-high-strength-suture#jnj-64e8f507470cb | |
| WilSuture | Rejoin Medical | 800648300 | For braided suture grafts |
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved