Method Article
Anterior Capsular Reconstruction with Human Dermal Allograft for Irreparable Subscapularis Tears
In This Article
Summary
This article details an open anterior capsular reconstruction technique using human dermal allograft for irreparable subscapularis tears, providing structural support and enhancing functional outcomes through precise graft fixation and rehabilitation.
Abstract
Anterior capsular reconstruction (ACR) using human dermal allograft (HDA) is an innovative surgical technique for managing irreparable subscapularis (SSc) tears. This procedure begins with patient positioning in the beach-chair configuration under general anesthesia, combined with an interscalene block for postoperative pain control. A deltopectoral approach is utilized, with an 8-10 cm incision extending from the coracoid tip to the deltoid tuberosity. After identifying and retracting the deltopectoral interval, the anterior glenoid is prepared by decorticating the bone surface to promote graft integration. Two suture anchors are placed at the 2- and 4-o'clock positions of the anterior glenoid. The HDA, measuring 50 mm × 40 mm and 3-4 mm in thickness, is folded into a double-layer configuration or used as a single layer based on the patient's requirements. The graft is secured with sutures to the glenoid anchors, with the arm positioned in neutral flexion, 30° abduction, and 30° external rotation for optimal tensioning. Additional fixation to the lesser tuberosity is achieved using a double-row suture bridge technique with anchors. For cases with a viable but retracted SSc tendon, augmentation over the graft is performed. Postoperative immobilization in an abduction brace is maintained for 6 weeks, followed by gradual rehabilitation. The precise graft fixation, tensioning, and structural support provided by this technique make ACR with HDA a valuable alternative to tendon transfers, preserving native shoulder biomechanics and offering a viable non-arthroplasty solution for severe anterior capsular deficiency.
Introduction
The subscapularis (SSc) is a critical component of the rotator cuff, responsible for maintaining shoulder stability, facilitating internal rotation, and acting as a restraint against anterior instability1. Damage or irreparable tears to the SSc can lead to significant pain, dysfunction, and progressive shoulder instability, often culminating in cuff tear arthropathy2. While surgical techniques such as tendon transfers are widely utilized to address these tears, they come with inherent limitations. Tendon transfers, including pectoralis major transfer, latissimus dorsi transfer, and latissimus dorsi with teres major transfers, are biomechanically non-anatomic and often fail to restore native shoulder kinematics, leading to high failure rates and complications3,4,5,6.
Anterior capsular reconstruction (ACR) with allograft has emerged as a promising alternative for managing irreparable SSc tears5,7. This technique offers a biomechanically anatomic solution by recreating the anterior capsule without compromising future surgical options8. It preserves shoulder biomechanics, providing a stable and functional joint environment8. The success of ACR has been inspired by the principles of superior capsule reconstruction, which have demonstrated improved outcomes in restoring shoulder stability in other rotator cuff pathologies9.
On the other hand, numerous studies have highlighted the effectiveness of human dermal allografts as augmentation in rotator cuff repair, with their clinical benefits also well-documented in superior capsular reconstruction9,10,11.
This technical note provides a comprehensive overview of the ACR technique using human dermal allografts to address irreparable SSc tears. By focusing on this specific technique, we aim to guide surgeons through the essential steps and considerations for successful ACR, emphasizing procedural nuances and the potential for improved clinical outcomes. This approach seeks to optimize functional recovery and pain relief for patients with severe SSc damage, offering a viable solution for those with limited treatment options.
Protocol
The protocol follows the guidelines of our institution's human research ethics committee.
1. Patient positioning and preparation
- Position the patient in a beach-chair configuration (Table of Materials) under general anesthesia to ensure optimal access to the shoulder joint.
- Administer an interscalene block for postoperative pain management.
NOTE: An interscalene block is performed by the anesthesiologist injecting a local anesthetic near the brachial plexus at the level of the anterior and middle scalene muscles. The procedure is guided by ultrasound to ensure accurate placement, providing targeted nerve blockades for shoulder and upper arm surgeries. - Prepare the surgical site using a standard sterile draping technique to expose the anterior shoulder region.
2. Surgical technique
- Approach and exposure
- Make an 8-10 cm deltopectoral incision, starting at the coracoid tip and extending distally toward the deltoid tuberosity (Figure 1).
- Identify the deltopectoral interval and retract the cephalic vein medially or laterally to protect it from damage.
- Incise the clavicopectoral fascia using electrosurgical pencils to expose the anterior joint capsule (Figure 2).
- Use retractors to maintain a clear surgical field and minimize trauma to surrounding structures (Figure 3).
- Subscapularis assessment and preparation
- Use a curette to create a bleeding bone surface on the humeral lesser tuberosity to enhance allograft integration (Figure 4).
- Mobilize the SSc tendon with sharp and blunt dissection to release adhesions.
- Visually evaluate the feasibility of a tension-free repair by assessing tendon quality and retraction.
- Proceed with anterior capsular reconstruction5 if the tendon is severely retracted or of poor quality.
- Glenoid preparation
- Insert a Fukuda retractor (Table of Materials) to improve the visibility of the glenoid (Figure 5).
- Decorticate the anterior glenoid surface at the 2- and 4-o'clock positions using a periosteal elevator, rasp, and curette to create a bleeding bone surface.
- Place two suture anchors (Table of Materials) at the prepared glenoid site for stable graft fixation (Figure 6).
- Graft preparation
- Select a human dermal allograft (Table of Materials) measuring approximately 50 mm × 40 mm and 3-4 mm thick.
- If additional thickness is required, fold the graft in half to create a double-layer construct. Folding is optional and at the surgeon's discretion.
- Reinforce the edges of the graft with 1-0 silk sutures for stability and ease of handling during fixation (Figure 7).
- Graft fixation
- Place two additional suture anchors (Table of Materials) into the humeral lesser tuberosity to secure the graft (Figure 8).
- Thread sutures from the glenoid anchors through the graft and secure it to the anterior glenoid with firm knotting (Figure 9 and Figure 10).
NOTE: In this illustrated case, the graft is not folded to increase its thickness. However, depending on the surgeon's preference, the graft can be folded to create a thicker construct. - Position the arm in neutral flexion with 30° of abduction and 30° of external rotation to ensure proper tensioning of the reconstructed capsule.
- Use sutures from the humeral lesser tuberosity anchors (Table of Materials) to pass through the graft (Figure 11). Secure the graft to the humeral side using a double-row suture bridge technique (Figure 12).
- Completion and augmentation
- If the SSc tendon stump is retracted but viable, suture it over the graft to augment the reconstruction.
- Close the rotator interval (Figure 13) and inferior capsule (Figure 14) using adjacent tissue sutures to restore the native soft tissue envelope.
3. Postoperative rehabilitation
NOTE: First-generation cephalosporins were administered as antibiotics until postoperative day 1. For pain management, NSAIDs were provided alongside opioids on a PRN basis. Opioids were administered when the postoperative pain visual analog scale (VAS) score exceeded 7.
- Immobilization phase
- Immobilize the shoulder in an abduction brace for 6 weeks to protect the reconstruction and facilitate initial healing.
- Initiate passive range-of-motion of forward flexion exercises during this period to prevent stiffness and maintain joint mobility without compromising graft fixation.
- Early rehabilitation phase
- At 6 weeks, begin a gradual rehabilitation program emphasizing passive and active-assisted range-of-motion exercises.
- Limit external rotation to 30° initially to avoid excessive stress on the graft.
- Strengthening phase
- Introduce isometric strengthening exercises at three months to rebuild muscle strength gradually.
- Progress to full active range of motion and advanced strengthening exercises by six months.
- Return to activity
- Gradually transition patients to daily activities and athletic pursuits after achieving adequate strength and stability.
Results
This retrospective study5 was conducted with institutional review board approval patients who underwent open ACR with human dermal allograft for irreparable SSc tears between August 2020 and January 2022.
A total of 18 patients (mean age: 63.7 years) underwent open anterior capsular reconstruction (ACR) using human dermal allografts for irreparable subscapularis (SSc) tears, with a mean follow-up of 17 months. Inclusion criteria included Yoo-Rhee type 4 or 5 tears, Goutallier stage ≥ 2 fatty infiltration, and Patte stage 3 tendon retraction. Postoperative rehabilitation involved immobilization for 6 weeks, passive range-of-motion exercises starting at 3 months, and return to full activity at 6 months. Human dermal allografts were folded into a double-layer construct for 17 patients, while a single-layer construct was used for one patient. Significant improvements were observed in clinical outcomes, with the visual analog scale (VAS) score decreasing from 6.6 ± 1.6 to 1.6 ± 1.5 (P < .001) and the University of California-Los Angeles (UCLA) shoulder score increasing from 12.4 ± 4.3 to 29.0 ± 4.5 (P < .001). Range of motion also improved notably, with forward flexion, abduction, and internal rotation at the side increasing by 28.6°, 32.5°, and 11.8°, respectively (P < .001). However, external rotation at the side decreased (P = .020). Successful graft healing occurred in 16 patients (88.9%), with two retears reported, both in patients who underwent double-layer anterior capsular reconstruction. Although 16 of 18 patients had healed graft at
the glenoid and humeral side, but there was no healing response between the layers when double layered graft was used.
Radiological outcomes showed improvements in coracohumeral distance (3.0 mm to 6.0 mm; P < .001) and increases in the acromiohumeral interval (8.1 mm to 8.8 mm; P = .070). No complications, such as stiffness, infections, or neurovascular injuries, were observed. However, the positive belly press sign remained postoperatively in 16 out of 18 patients (p=.480). These findings suggest that open ACR with human dermal allografts can significantly enhance clinical and radiological outcomes for irreparable SSc tears while maintaining a low complication rate. The surgical details of the study are summarized in Table 1.

Figure 1: Deltopectoral incision. An 8-10 cm deltopectoral incision is made starting at the coracoid tip and extending distally toward the deltoid tuberosity. This incision provides access to the anterior shoulder structures. Please click here to view a larger version of this figure.

Figure 2: Clavicopectoral fascia exposure. The clavicopectoral fascia is incised to expose the anterior joint capsule. Please click here to view a larger version of this figure.

Figure 3: Retractor placement. Retractors are used to maintain a clear surgical field, minimizing trauma to surrounding soft tissues and improving visibility during anterior capsular reconstruction. Please click here to view a larger version of this figure.

Figure 4: Humeral lesser tuberosity preparation. A curette is utilized to decorticate the humeral lesser tuberosity, creating a bleeding bone surface to enhance the integration of the human dermal allograft. Please click here to view a larger version of this figure.
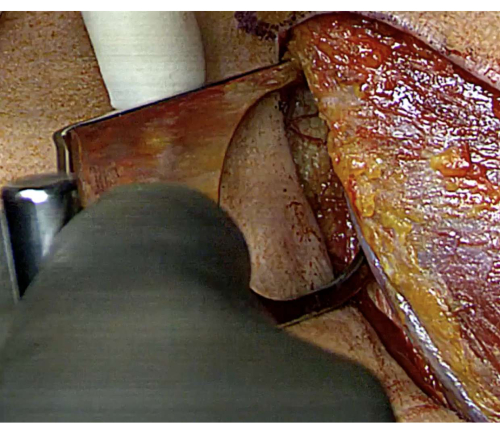
Figure 5: Glenoid exposure with a Fukuda retractor. A Fukuda retractor is inserted to improve visualization of the anterior glenoid, aiding in accurate preparation for graft fixation. Please click here to view a larger version of this figure.
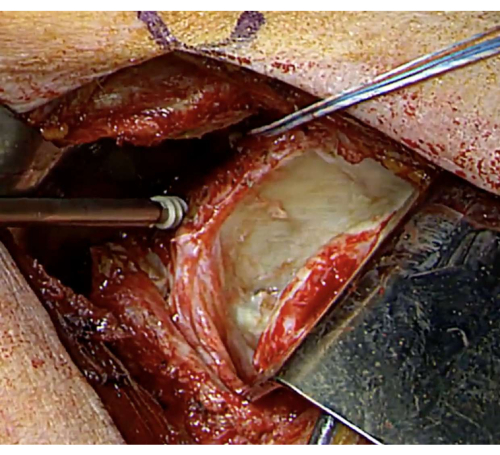
Figure 6: Anterior glenoid anchor fixation. The anterior glenoid surface is decorticated at the 2- and 4-o'clock positions using a periosteal elevator, and place two suture anchors at the prepared glenoid site for stable graft fixation Please click here to view a larger version of this figure.
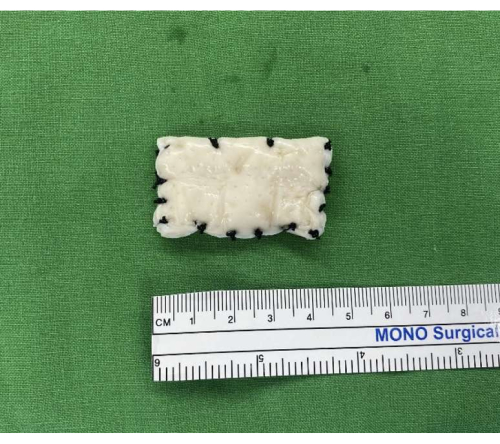
Figure 7: Human dermal allograft preparation. A human dermal allograft measuring 50 × 40 mm and 3-4 mm in thickness is prepared. The edges are reinforced with silk sutures for stability and ease of handling during fixation. Please click here to view a larger version of this figure.

Figure 8: Suture anchor placement on humeral lesser tuberosity. Two suture anchors are inserted into the humeral lesser tuberosity, providing a secure base for graft fixation to the humeral side. Please click here to view a larger version of this figure.

Figure 9: Suture passing through graft. Sutures from glenoid anchors are threaded through the human dermal allograft, securing it to the anterior glenoid surface with firm knotting. Please click here to view a larger version of this figure.

Figure 10: Graft fixation on the glenoid. The human dermal allograft is firmly secured to the anterior glenoid, with precise positioning to ensure stability and optimal tension. Please click here to view a larger version of this figure.

Figure 11: Suture passage for humeral fixation. Sutures from the humeral anchors are passed through the graft for secure fixation, preparing for the final double-row suture bridge technique. Please click here to view a larger version of this figure.

Figure 12: Double-row suture bridge technique. The graft is anchored to the humeral lesser tuberosity using a double-row suture bridge technique, ensuring robust fixation on the humeral side. Please click here to view a larger version of this figure.
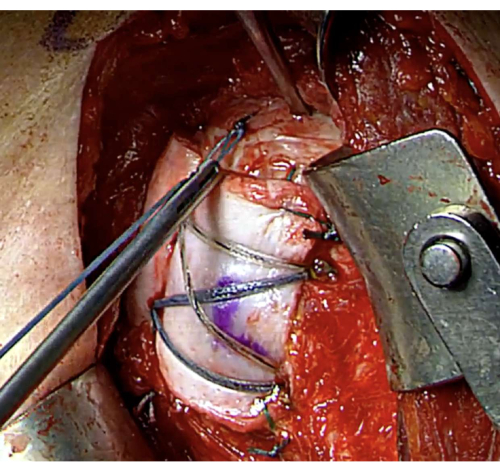
Figure 13: Rotator interval closure. The rotator interval is closed using adjacent tissue sutures to restore the native soft tissue envelope, enhancing joint stability. Please click here to view a larger version of this figure.

Figure 14: Inferior capsule closure. The inferior capsule is sutured to adjacent tissues, completing the reconstruction and reinforcing the shoulder's anatomical structure Please click here to view a larger version of this figure.
Table 1: Surgical details of the study. Please click here to download this Table.
Discussion
The success of ACR with human dermal allograft is contingent upon meticulous surgical technique and adherence to key procedural steps. Accurate preparation of the anterior glenoid and the lesser tuberosity of the humerus is crucial to achieve optimal fixation and facilitate graft integration. Proper tensioning of the reconstructed capsule is equally critical and is accomplished by positioning the arm in neutral flexion with 30° of abduction and 30° external rotation during the procedure. Postoperative rehabilitation plays a pivotal role in ensuring graft healing and long-term functional outcomes. A gradual and stepwise rehabilitation protocol, rather than an overly aggressive approach, is recommended to support graft incorporation and minimize the risk of complications. Adhering to these principles is essential for maximizing the clinical success of ACR with human dermal allograft5,12.
The method demonstrated some limitations. First, the lack of healing between layers in double-layer constructs suggests a need for further refinement in graft design or surgical technique. Additionally, despite improvements in pain and function, a persistent positive Belly Press Sign in 88.9% of patients indicates incomplete restoration of SSc function.
Compared to alternative techniques such as pectoralis major or latissimus dorsi tendon transfers, ACR with human dermal allograft offers significant biomechanical advantages. Tendon transfers have inherent limitations, including their non-anatomic nature and less predictable outcome13. these procedures are associated with notable retear rates and complications, such as injuries to the musculocutaneous or axillary nerves14,15. Unlike tendon transfers, which often result in non-physiologic muscle activation, ACR provides a more natural restoration of shoulder biomechanics16. Furthermore, this method preserves the option for future salvage procedures, such as reverse total shoulder arthroplasty, if necessary.
The findings from this study highlight the potential of ACR with human dermal allograft as a promising treatment for irreparable SSc tears, particularly in patients who are not candidates for arthroplasty or tendon transfers. The technique's ability to reduce pain, improve range of motions, and restore shoulder stability makes it a valuable option for managing challenging rotator cuff pathologies. Future research could explore the long-term outcomes of this method and its application in younger, more active patient populations. Additionally, advancements in graft materials and surgical techniques could expand its applicability to other shoulder instability conditions, further enhancing its clinical utility.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors have no acknowledgment.
Materials
| Name | Company | Catalog Number | Comments |
| Lift-Assist Beach Chair Positioner | Arthrex, Naples, FL, USA | AR-1627 | Surgical bed |
| Universal Head Positioner | Arthrex, Naples, FL, USA | AR-1627-05 | Head holder |
| SPIDER2 | Smith & Nephew, Watford, UK | 72203299 | Pneumatic arm holder |
| HEALICOIL | Smith & Nephew, Watford, UK | 72203707 | Anchors for glenoid |
| Hi-Fi Tape | CONMED, Utica, NY, USA | YRC03 | Anchors for humerus, medial row |
| CrossFT | CONMED, Utica, NY, USA | CFK-55DT | Anchors for humerus, |
| Knotless DT | CONMED, Utica, NY, USA | CFK-55DT | lateral row |
| Electrosurgical Pencils | CONMED, Utica, NY, USA | 131307A | Electrocauterization |
| BellaCell HD | Hans, Daejeon, Korea | Not applicable | Human dermal allografts |
| Modified Fukuda-type Retractor | Innomed, Savannah, GA, USA | 1930 | Retractor for optimizing the surgical view of the glenoid |
References
- Meshram, P., Rhee, S. M., Park, J. H., Oh, J. H. Comparison of functional and radiological outcomes of tears involving the subscapularis: Isolated subscapularis versus combined anterosuperior rotator cuff tears. Orthop J Sports Med. 8 (2), 2325967119899355 (2020).
- Su, W. -. R., Budoff, J. E., Luo, Z. -. P. The effect of anterosuperior rotator cuff tears on glenohumeral translation. Arthroscopy. 25 (3), 282-289 (2009).
- Elhassan, B. T., Wagner, E. R., Kany, J. Latissimus dorsi transfer for irreparable subscapularis tear. J Shoulder Elbow Surg. 29 (10), 2128-2134 (2020).
- Luo, Z., et al. Outcome comparison of latissimus dorsi transfer and pectoralis major transfer for irreparable subscapularis tendon tear: A systematic review. Am J Sports Med. 50 (7), 2032-2041 (2022).
- Rhee, Y. G., Kyeong, T. H., Rhee, S. M., Kantanavar, R. Anterior capsular reconstruction in irreparable subscapularis tear: human dermal allograft. J Shoulder Elbow Surg. 32 (11), 2256-2263 (2023).
- Baek, C. H., Kim, J. G., Baek, G. R. Outcomes of combined anterior latissimus dorsi and teres major tendon transfer for irreparable anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 31 (11), 2298-2307 (2022).
- Pogorzelski, J., Hussain, Z. B., Lebus, G. F., Fritz, E. M., Millett, P. J. Anterior capsular reconstruction for irreparable subscapularis tears. Arthrosc Tech. 6 (4), e951-e958 (2017).
- Omid, R., et al. Biomechanical analysis of anterior capsule reconstruction and latissimus dorsi transfer for irreparable subscapularis tears. J Shoulder Elbow Surg. 29 (2), 374-380 (2020).
- Mihata, T., et al. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 44 (6), 1423-1430 (2016).
- Nuvoli, N., et al. Biological patch in the repair of rotator cuff tears: Functional and clinical evaluation of twenty-three cases with a mean follow-up of six years. J Clin Med. 13 (18), 5596 (2024).
- Russo, M., Dirkx, G. K., Rosso, C. Patch augmentation in arthroscopic rotator cuff surgery-review of current evidence and newest trends. J Clin Med. 13 (17), 5066 (2024).
- Mirzayan, R., Korber, S. Anterior capsular reconstruction with acellular dermal allograft for subscapularis deficiency: a report of two cases. Clin Shoulder Elb. 27 (1), 126-130 (2024).
- Shin, J. J., et al. Pectoralis major transfer for treatment of irreparable subscapularis tear: a systematic review. Knee Surg Sports Traumatol Arthrosc. 24 (6), 1951-1960 (2016).
- Elhassan, B., et al. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work. J Bone Joint Surg Br. 90 (8), 1059-1065 (2008).
- Ruiz-Ibán, M. A., Murillo-González, J. A., Díaz-Heredia, J., Avila-Lafuente, J. L., Cuéllar, R. Pectoralis major transfer for subscapular deficiency: anatomical study of the relationship between the transferred muscle and the musculocutaneous nerve. Knee Surg Sports Traumatol Arthrosc. 21 (9), 2177-2183 (2013).
- Komperda, K. W., et al. Anterior Capsule reconstruction versus pectoralis major transfer for irreparable subscapularis tears involving the anterior capsule: A comparative biomechanical cadaveric study. Arthroscopy. 35 (11), 3002-3008 (2019).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved