Method Article
Application of the Downward-Turned Patch-Wrapped Prosthesis Method in Transaxillary Single-Port Endoscopic Breast Reconstruction
In This Article
Summary
We present a protocol using a single-port endoscopic approach with immediate breast reconstruction for breast cancer. The patch manipulation technique involves wrapping the prosthesis for protection, demonstrating safety and advantages over traditional methods.
Abstract
This study presents an innovative breast reconstruction technique using an axillary single-port endoscopic approach with immediate breast reconstruction for breast cancer. The procedure begins with a concealed incision along the axillary fold that serves as a sentinel lymph node biopsy and endoscopic access. Under high-definition endoscopic visualization, meticulous dissection of the posterior space of the pectoralis major muscle and the retromammary space is performed, preserving critical neurovascular structures. A unique subcutaneous tunneling technique using long curved scissors enables the thorough separation of the breast parenchyma from the subcutaneous tissues, facilitating the en bloc resection of the mammary glands. The nipple-areolar complex was subjected to intraoperative frozen section analysis to confirm margin clearance. A critical step involves expertly folding and turning the patch upward before inserting it along the free edge of the pectoralis major muscle, where it is secured in place through continuous suturing. Surgical innovation is centered on patch manipulation protocols. The prosthesis is meticulously wrapped in a downwardly positioned patch to ensure complete enclosure and protection. The findings of this study strongly suggest that this single-port axillary endoscopic radical mastectomy, complemented by an innovative downward patch-wrapping technique, represents an effective and superior approach for the treatment of breast cancer, providing favorable outcomes and improved recovery experiences. This procedure was successfully performed in 30 patients at our hospital, with an average operating time of 147.73 min and a mean follow-up period of 17 months, and the BREAST-Q score post-operation was higher than that of pre-operation. These results indicate significant advantages over traditional reconstruction methods regarding aesthetic outcomes and postoperative recovery.
Introduction
Breast cancer is the most prevalent malignancy among women worldwide1. Owing to advancements in comprehensive treatment strategies, patient prognosis has significantly improved, resulting in higher survival rates and an increased emphasis on aesthetic outcomes2. However, breast resection may result in physical disfigurement, a diminished sense of femininity, and psychological distress, including postoperative anxiety and depression. The subsequent decline in self-confidence may further contribute to sexual dysfunction and strains in marital and interpersonal relationships.
The surgical treatment of breast cancer has evolved from an initial focus on radical excision to a more holistic approach that prioritizes nipple-areolar complex preservation and breast reconstruction. Although breast-conserving surgery is an excellent option3,4, it may not be suitable for patients with larger tumors, multiple or suspicious cancer lesions, or microcalcifications5. Additionally, due to the typically smaller breast size among Chinese women, postoperative asymmetry is frequently observed following breast-conserving surgery6. The requirement for postoperative radiotherapy further complicates the decision-making process. Consequently, many patients, particularly those with stage I or II breast cancer, opt to undergo breast reconstruction surgery7. However, traditional reconstruction methods often result in visible scars due to incisions made on the breast surface.
In recent years, double-planar breast reconstruction following pectoral muscle reconstruction has attracted attention as an emerging technique. This approach not only improves the aesthetic outcomes of breast reconstruction but also alleviates postoperative pain and discomfort to a certain extent, particularly in patients with poor skin quality8. Additionally, post-pectoral biplanar reconstruction has been shown to reduce the incidence of postoperative muscle contractions and motor dysfunction, especially in patients undergoing radiotherapy9.
In post-pectoral prosthesis breast reconstruction, the use of patches helps improve postoperative outcomes. Studies have shown that patches can significantly reduce the incidence of postoperative complications, such as infection and capsule contracture10. In addition, their use can improve the aesthetic outcomes of breast reconstruction and help patients regain their self-confidence and body image11,12.
The traction-line parachute method is used to wrap the prostheses using patches due to its low complication rate and good aesthetic effect. However, this method is complicated, resulting in prolonged surgical time, especially for inexperienced surgeons. To address this challenge, surgical modifications were implemented by continuously suturing the patch to the lower edge of the pectoralis major and turning its lower edge upward. After inserting the prosthesis, the natural arc of the prosthesis was followed, and the patch was turned down again to fully enclose the prosthesis. These refinements simplified the procedure and reduced the surgical time.
Patients underwent a single-port axillary endoscopic radical mastectomy with implant-based reconstruction of the pectoralis muscle. Comprehensive data were collected from the 30 patients included in the analysis. The inclusion criteria included patients: (1) who were aged 20-65 years; (2) had a tumor maximum diameter of ≤5.0 cm or ≤5.0 cm after neoadjuvant chemotherapy; (3) whose preoperative magnetic resonance imaging confirmed the absence of invasion in the nipple-areola complex, skin, or pectoralis major muscle or distant metastases; (4) whose preoperative core needle biopsy confirmed the presence of a breast malignant tumor; (5) who had an Eastern Cooperative Oncology Group performance status score of 0-2; and (6) who showed willingness to undergo breast reconstruction.
By contrast, patients: (1) with large breast volume or significant ptosis, preventing surgery owing to insufficient breast volume or a relatively symmetrical appearance through simple implantation; (2) whose preoperative examination or intraoperative rapid pathological examination showed tumor invasion of the nipple-areola complex, skin, or pectoralis major muscle; or (3) with clinical stage IIIB or later tumors prior to surgery were excluded.
Protocol
A retrospective analysis of clinical data was conducted at Ningxia Medical University General Hospital between August 2020 and March 2023. This study was approved by the Medical Research Ethics Review Committee of the General Hospital of Ningxia Medical University (KYLL-2021-915). All procedures were performed in accordance with established regulations and ethical guidelines.
1. Identification of the presence of breast cancer through immunohistochemical (IHC) staining
NOTE: The human epidermal growth factor receptor 2 (HER2) overexpression is shown in Figure 1. The overexpression of HER2 significantly impacts the treatment of breast cancer.
- Obtain breast tissues using hollow needle biopsy and immerse them immediately in a 10% neutral-buffered formalin fixative.
- Send the tissues to the pathology department for IHC staining by professional pathologists to determine the pathological type of breast cancer.
NOTE: Follow the IHC staining steps described in previous studies13.
2. Selection of appropriate prosthesis according to breast size, tumor characteristics, and personal preference
NOTE: The SN indicates the distance from the midpoint of the sternal notch to the nipple, whereas NN indicates the distance between the two nipples, and SN-NN means SN minus the NN. Endoscopic implant breast reconstruction does not require reducing the convexity or volume of the prosthesis, as the incision is away from the tension zone caused by the prosthesis.
- Measure the distance from 1.5-2.0 cm beside the midline to the anterior axillary line using a caliper. Identify this as the maximum basal diameter of the breast (X). Measure the thickness of the outer soft tissue (Y) and inner soft tissue (Z) of the breast. Lastly, calculate the basal diameter of the implant as X − (Y/2 + Z/2).
- Select the height of the prosthesis according to the distance of SN-NN. Choose a medium-height prosthesis if the SN-NN distance is between 0 cm and 2 cm. Choose a low-height prosthesis if the SN-NN distance is less than 0 cm. Choose a full or extra-full prosthesis if the SN-NN distance is greater than 2 cm.
- Use a full convex prosthesis in breasts with significant ptosis or skin laxity; otherwise, use a medium or low-sized prosthesis.
NOTE: The degree of ptosis in postoperative patients is shown in Supplementary Figure 1.
3. Planning for endoscopic breast reconstruction
- Inform patients about the risks and potential complications, including changes in the surgical procedure, skin flap necrosis, incision dehiscence, incision infection, and capsular contracture.
- After obtaining informed consent, administer a low-molecular-weight heparin calcium injection (100 AXaIU/kg) for perioperative thrombosis prophylaxis 1 day prior to the surgery.
- Administer one dose of intravenous cefazolin sodium (1 g) 30 min before surgery to prevent infection.
NOTE: Administer an additional dose if the surgery lasts more than 3 h and another dose 6 h after surgery. - Administer general anesthesia with endotracheal intubation by an anesthesiologist. Place the patient in a supine position, raise the affected shoulder 25° with a shoulder pad, and abduct the upper arm 60° for proper surgical positioning (Figure 2). Monitor vital signs continuously.
- Inject anesthetic drugs (propofol or remifentanil) slowly via intravenous infusion to induce gradual loss of consciousness. Administer muscle relaxants, such as rocuronium, to facilitate tracheal intubation.
- Once loss of consciousness and muscle relaxation are achieved, use a laryngoscope to expose the glottis, insert the tracheal tube into the trachea, and connect the anesthesia machine for mechanical ventilation.
4. Downward-turned patch-wrapped prosthesis method in transaxillary single-port endoscopic breast reconstruction
- Perform sentinel lymph node biopsy (SLNB).
- Inject 2 mL of methylene blue into the nipple-areola complex of the affected side 10 min prior to the surgery.
- Make a concealed incision (approximately 6 cm) in the axillary fold, dissect the subcutaneous tissue, and perform SLNB at the outer edge of the pectoralis major muscle.
- Identify the blue-dyed lymphatic vessels and trace them to locate the stained lymph nodes, the sentinel lymph nodes.
- Dissect and completely remove the sentinel lymph nodes to avoid rupturing the lymph nodes or damaging the surrounding tissues.
- Send the excised sentinel lymph nodes to the pathology department for rapid pathological analysis to determine the presence of tumor metastasis. If SLNB is positive, perform axillary lymph node dissection.
- Separate the posterior intercostal muscles.
- Insert an incision protector through the axillary incision and place a rolled-up #6.5 glove inside the protector.
- Place the puncture devices 5 mm, 12 mm, and 5 mm into the thumb, middle finger, and little finger of the glove, respectively (Figure 3).
- Insert a suction catheter (16 #) into the glove's index finger to prevent smoke accumulation.
- Separate the subcutaneous tissue and fascia to expose the space behind the pectoralis major muscle.
- Use a suction device to push the pectoralis major muscle upward to create a roof like space.
- Use an ultrasonic scalpel to sharply dissect and separate the pectoralis major muscle posterior space.
- The pectoralis major muscle has multiple attachment points on ribs three to five. When separating these muscle attachment points, cut the muscle in situ and coagulate the blood vessels to prevent bleeding. Maintain the cavity with CO2 insufflation at a pressure of 10-12 mmHg.
- Separate the posterior breast gap.
- Determine the separation range before surgery based on the breast boundary marking point, generally exceeding the marking point by 1 cm.
- If the breast is significantly ptosis, extend the lower edge beyond the marking point by 2-3 cm, from the subclavian to the anterior sheath of the rectus abdominis and from the sternum to the fusion fascia.
- Push the breast gland upward to expose the facial surface of the pectoralis major muscle.
- Use an electrocoagulation hook to cut the loose tissue between the breast gland and the pectoralis major muscle.
- Slow down when approaching the inner edge of the rib to prevent bleeding.
- Coagulate and cut the blood vessels larger than 3 mm using an ultrasonic scalpel to prevent bleeding.
- Determine the separation range before surgery based on the breast boundary marking point, generally exceeding the marking point by 1 cm.
- Separate the subcutaneous tissue using the tissue scissor tunnel method.
NOTE: As the blood vessels from the intercostal space have already coagulated in the previous steps, the risk of subcutaneous bleeding is low. Therefore, tissue scissors are used to separate the subcutaneous tissue.- Inject 100-150 mL of swelling fluid subcutaneously to create a subcutaneous space under the skin owing to the expansion and fat-dissolving effects of the liquid.
NOTE: The swelling fluid contains 1:500,000 adrenaline and 20 mL of lidocaine hydrochloride. - Insert tissue scissors into the subcutaneous space to establish four subcutaneous tunnels and expand them using the scissor head.
- Use the tissue scissors to sharply separate the subcutaneous tissue (0.5 cm) inside the glandular edge along the established tunnels, including the tissue below the nipple and areola.
- Gradually connect the four subcutaneous tunnels to form a continuous subcutaneous space.
- Inject 100-150 mL of swelling fluid subcutaneously to create a subcutaneous space under the skin owing to the expansion and fat-dissolving effects of the liquid.
- Remove the breast glands completely.
NOTE: The connection between the gland and skin consists of a small amount of tissue around the gland as the subcutaneous space of the breast and posterior breast gap have already been separated.- Carefully place the endoscope along the puncture devices.
- Maintain the CO2 pressure at 8 mmHg.
- Use ultrasonic or electric scalpels to cut, separate the natural arc of the gland formed by CO2 pressure, and completely remove the gland.
- Achieve thorough hemostasis and rinse the wound with 1,000 mL of distilled water at 42 °C.
- Collect tissue samples from four points on the nipple-areola complex and send them for rapid pathological examination during surgery.
- Preserve the nipple if no carcinoma cells are present at the nipple resection margin; otherwise, remove the nipple if carcinoma cells are detected at the incision margin.
NOTE: Pathology reports are provided by professional pathologists.
- Cut the lower and inner edges of the pectoralis major.
- Separate the anterior and posterior gaps of the pectoralis major.
- Use an ultrasonic scalpel to cut along the lower edge of the pectoralis major toward the inner edge and cut the inner edge close to the fourth rib.
- Suture the patch.
- Fold the patch in half, flip up the lower edge, and suture the inner edge using a 3-0 absorbable suture
- Insert the patch along the free edge of the pectoralis major and flatten it.
- Suture the patch to the lower and inner free edges of the pectoralis major.
- Wrap the prosthesis with a downward patch.
- Insert the prosthesis under the patch and wrap it downward.
- Push the outer patch toward the back and upper parts of the prosthesis, and push the lower patch toward the inner upper part repeatedly using an oval clamp until the patch completely wraps the prosthesis along the edge of the outer prosthesis.
- Compare both sides and perform shaping.
- Place a 15# high negative pressure drainage tube in the axilla and below the crease of the breast on each side.
5. Management after surgery
- Collect the necessary data, including surgical time, length of hospital stay, costs, drain output post-surgery, body mass index, and tumor size.
- Record and evaluate associated complications, including incision infection, flap necrosis, incision dehiscence, implant removal, and patient satisfaction score after reconstruction.
- Perform follow-up of patients every 3 months after surgery.
- Conduct physical examinations, ultrasound, positron emission tomography-computed tomography (PET-CT), and other examinations for suspected metastases.
- Evaluate treatment compliance, recurrence or distant metastasis, and breast appearance using BREAST-Q (breast cancer module).
6. Data analysis.
- Use appropriate statistical software to analyze the data. Express normally distributed quantitative data as mean ± standard deviation, whereas non-normally distributed quantitative data as the median (interquartile range).
- Express categorical data as frequencies and percentages.
Results
General patient data
Patient characteristics are listed in Table 1. The analysis included 30 female patients with a mean age of 43.17 years and a mean body mass index of 23.04 kg/m2. The average tumor diameter was 1.77 cm. The TNM stages were as follows: stage 0, 3 patients; stage I, 15 patients; stage II, 11 patients; and stage III, 1 patient.
SLNB was performed in all patients, with an average of 9.43 axillary lymph nodes examined. An axillary lymph node dissection was performed in 11 patients (36.67%) based on the patient's clinical condition. The surgical time ranged from 55-420 min, with an average duration of 147.73 min. The average length of hospital stay was approximately 8 days, whereas the average postoperative discharge time was 2.2 days.
Postoperative complications and follow-up
Five patients (16.6%) developed postoperative complications, including two with incision infection, one with incision dehiscence, one with incision infection and dehiscence, four with incision, and one patient experienced incision infection, dehiscence, and flap necrosis. The prosthesis was finally removed due to radiation dermatitis following postoperative radiotherapy. All 30 patients were followed up for 3 months postoperatively, and none of them experienced recurrence, metastasis, or death. However, incision dehiscence and infection negatively affected drainage and patient satisfaction.
The average total drainage volumes were 285.04 mL in patients without incision dehiscence and 491.67 mL in patients without incision infection, significantly lower than in patients with incision dehiscence and incision infection. Moreover, breast satisfaction scores were notably higher in patients without incision dehiscence or incision infection (Table 2 and Table 3).
The breast satisfaction scores showed no significant differences (approximately 70) across various TNM stages (Table 4). The breast satisfaction scores after surgery (71.9) were significantly higher than those before surgery (64.58) (Table 5). The median follow-up time was 512.5 days (Table 6).

Figure 1: Preoperative histopathological results. A representative image of HER2-overexpressing breast cancer. Scale bar: 10 µm. Please click here to view a larger version of this figure.

Figure 2: Surgical incision and patient positioning for stage I breast reconstruction using an axillary single-hole endoscopic prosthesis. The white arrow pointed to the incision. Please click here to view a larger version of this figure.
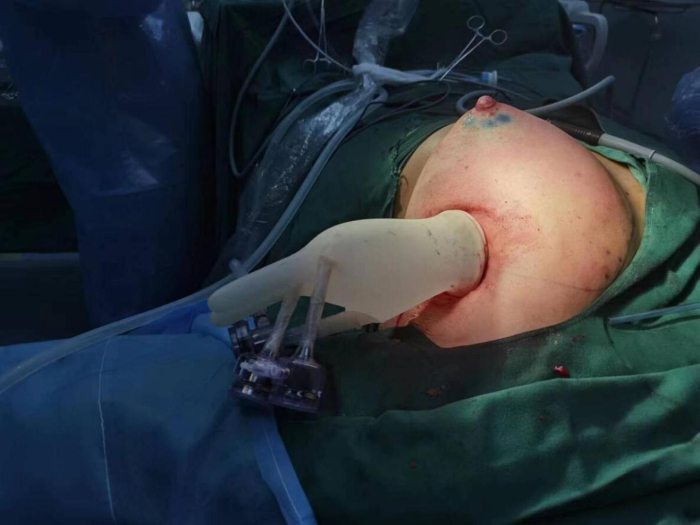
Figure 3: Trocar insertion for stage I breast reconstruction using an axillary single-hole endoscopic prosthesis. Please click here to view a larger version of this figure.
| Indicators | Statistic | |
| Age at surgery (years) | 43.17 ± 8.65 | |
| Height (M) | 1.61 ± 0.04 | |
| Weight (kg) | 59.95 ± 6.35 | |
| BMI (kg/m2) | 23.04 ± 2.36 | |
| Tumor diameter (cm) | 1.77 ± 0.88 | |
| pTNM | Phase 0 | 3 (10.00%) |
| Phase I | 15 (50.00%) | |
| Phase II | 11 (36.67%) | |
| Phase III | 1 (3.33%) | |
| Examination of axillary lymph node | 9.43 ± 7.27 | |
| Axillary lymph node metastasis | 0.57 ± 1.07 | |
| Axillary lymph node dissection | Yes | 11 (36.67) |
| No | 19 (63.33) | |
| Surgical duration (min) | 147.73 ± 60.38 | |
| Hospitalization days | 8.00 ± 5.68 | |
Table 1: General clinical data of 30 patients.
| Incision dehiscence | ||
| No (n = 27) | Yes (n = 3) | |
| First day total drainage (mL) | 132.96 ± 60.12 | 225 ± 101.49 |
| Second day total drainage (mL) | 103.26 ± 51.41 | 193.33 ± 103 |
| Third day total drainage (mL) | 50.69 ± 56.62 | 73.33 ± 64.29 |
| Total drainage (mL) | 285.04 ± 122.37 | 491.67 ± 267.32 |
| Breast satisfaction score | 73.94 ± 5.88 | 61.33 ± 7.09 |
| Medical service satisfaction score | 83.15 ± 17.88 | 46.67 ± 11.55 |
| Psychosocial health score | 75.31 ± 6.31 | 64 ± 6 |
| Physical health score | 78.93 ± 8.2 | 75.83 ± 6.51 |
| Sexual health score | 79.67 ± 10.65 | 64 ± 14.42 |
Table 2: Incision dehiscence and patient satisfaction.
| Incision infection | ||
| No (n = 26) | Yes (n = 4) | |
| First day total drainage (mL) | 129.23 ± 58.03 | 226.25 ± 82.9 |
| Second day total drainage (mL) | 98.38 ± 45.62 | 202.5 ± 86.07 |
| Third day total drainage (mL) | 49.15 ± 57.46 | 86.67 ± 41.63 |
| Total drainage (mL) | 276.77 ± 116.85 | 493.75 ± 218.3 |
| Breast satisfaction score | 74.44 ± 4.71 | 61.25 ± 9.46 |
| Medical service satisfaction score | 84.81 ± 13.82 | 45 ± 25.17 |
| Psychosocial health score | 75.67 ± 5.75 | 64.5 ± 8.06 |
| Physical health score | 78.96 ± 8.44 | 76.38 ± 4.4 |
| Sexual health score | 81.04 ± 9.53 | 59 ± 5.03 |
Table 3: Incision infection, patient satisfaction, and drainage volume.
| Stage | n | Breast satisfaction scores ( ) ) | |
| T | 1 | 22 | 71.82 ± 7.71 |
| 2 | 8 | 75.06 ± 4.12 | |
| N | 0 | 21 | 74.31 ± 5.75 |
| 1 | 8 | 67.56 ± 8.06 | |
| 2 | 1 | 79.50 ± 0.00 | |
| M | 0 | 30 | 72.68 ± 7.02 |
Table 4: Analysis of breast satisfaction scores and TNM staging.
| Before surgery | After surgery | Difference | |
| Breast satisfaction score | 64.58 ± 10.93 | 71.9 ± 7 | 7.32 ± 15.24 |
| Psychosocial health score | 69.28 ± 11.25 | 73.33 ± 7.21 | 4.05 ± 16.29 |
| Physical health score | 71.07 ± 10.64 | 78.47 ± 8.25 | 7.4 ± 15.22 |
| Sexual health score | 66.67 ± 9.36 | 77.02 ± 11.95 | 10.35 ± 16.95 |
Table 5: Analysis of breast satisfaction scores before and after surgery.
| Percentiles | Day |
| P25 | 117 |
| P50 | 512.5 |
| P75 | 820.75 |
Table 6: Follow-up duration.
Supplementary Figure 1. Breast ptosis post-surgery. (A) No ptosis. (B) Mild ptosis. (C) Moderate ptosis. Please click here to download this File.
Discussion
Breast reconstruction has become a vital element in enhancing the quality of life of patients undergoing extensive breast cancer surgery. Regarding prosthetic-based reconstruction, the utilization of patches is essential to ensure prosthesis stability and achieve an optimal aesthetic outcome14,15. Although the use of traditional traction-line parachutes in pediatric breast reconstruction presents certain benefits, prolonging the surgical duration has become a significant challenge in clinical practice16. This method requires multiple sutures around the patch, functioning in a manner similar to the pull thread of a parachute to enclose the prosthesis17. By tugging on these lines, the prosthesis is enclosed18. However, this approach has certain limitations. The suture traction is directed toward the armpit, whereas the patch must wrap the prosthesis inward. This directional contradiction complicates patch placement and extends the surgical time. Additionally, the complexity of the procedure and the surgeon's experience significantly influence the duration of surgery19. Less experienced surgeons often require more time to master the technical aspects of the traction-line parachute method, further prolonging the surgical time. Thus, optimizing the surgical process and reducing the surgical time have become the primary objectives of this study.
This technique consists of two essential steps. First, the patch is sutured to the lower edge of the pectoralis major muscle after prosthesis reconstruction following the completion of radical breast cancer. Continuous suturing with absorbable threads is used, eliminating unnecessary steps and significantly reducing surgical time compared with traditional techniques. Second, the prosthesis is implanted behind the pectoralis major muscle, and the patch is guided downward along the natural arc of the prosthesis to achieve an impeccable wrap.
During prosthesis placement, precise positioning of the prosthesis is crucial for successful reconstruction. However, multiple suture fixations make adjusting the prosthesis position challenging. Research has indicated that traction lines may cause prosthesis shifting during implantation, adversely affecting the reconstruction outcome20. Furthermore, the surgeon's assessment of prosthesis positioning during the procedure depends on experience, clarity of the surgical field, and anatomical variations. Therefore, enhancing the accuracy of prosthesis positioning and reducing the likelihood of postoperative complications remain the key areas of investigation. In this technique, the prosthesis is positioned and then wrapped and secured once it reaches a predetermined location. Compared with traditional surgical methods, this approach allows for easier adjustment of the prosthesis position and more precise placement.
Moreover, ensuring patch flatness is a critical consideration. Research has indicated that postsurgical patch wrinkles or unevenness can not only affect aesthetics but also contribute to the development of postoperative complications21. Several factors influence patch flatness, including the surgeon's skill level, patch material properties, and postoperative care22. Consequently, ensuring a flatter patch application is essential. In this technological enhancement, we utilized direct visualization and a downward wrapping technique for the prosthesis. Under direct endoscopic vision, we initially wrapped the lateral prosthesis along its natural arc, ensuring a smooth and even application. Subsequently, the outer wrapping line was followed to enclose the lower edge of the prosthesis. Finally, an endoscopic examination was conducted, and necessary adjustments were made to ensure uniform wrapping. This technique, performed under direct observation, is simple and precise.
Furthermore, suturing the patch to the pectoralis major muscle is a critical step in the procedure. The sutures must not only secure the patch and pectoralis major but also prevent injury to the pectoralis major muscles. Research has demonstrated that the use of Vicryl threads for continuous suturing is associated with lower complication rates and higher patient satisfaction during postoperative recovery23. During the undercut patch wrapping of the prosthesis, the application of the continuous suture technology provides considerable advantages. First, the Vicryl thread exhibits excellent biocompatibility and tensile strength, facilitating a smoother suturing process while reducing the risk of postoperative infection. Second, continuous suturing effectively disperses tension, minimizes damage to local tissues, and reduces the likelihood of pectoral muscle tearing. No instances of pectoral muscle tears or prosthesis displacement were observed in any patient.
Assessment of postoperative aesthetics is a crucial metric in breast reconstruction surgery, as they are closely linked to a patient's quality of life. Aesthetic outcomes can significantly impact a patients' self-esteem, social interactions, and psychological well-being. The shape of the prosthesis affects the aesthetics of post-reconstruction surgery. The prosthesis is mainly divided into circular and anatomical (i.e., water drop shape). The circular prosthesis is relatively round and full shape; the water droplet-shaped prosthesis simulates the shape of the natural breast when standing, with the upper half slightly flattering and the lower half being plump and more in line with the natural breast shape of the human body24. Studies have shown that the satisfaction score and overall quality of life of water droplet-shaped prosthesis are significantly higher than that of circular prosthesis10,25 . Therefore, all the prostheses placed in this study were water droplet-shaped, and the aesthetics were evaluated through the BREAST-Q questionnaire25. Through professional evaluation, a comprehensive understanding of the postoperative outcomes can be achieved, serving as a foundation for clinical decision-making. The mean breast satisfaction score of the patients 3 months after surgery exceeded 70 points, which was markedly higher than those reported in other studies26.
In summary, the laparoscopic radical mastectomy and breast reconstruction technique using the axillary single-hole approach has demonstrated promising outcomes in the radical treatment and aesthetic shaping of breast cancer. The downward prosthesis wrapping method is easy to perform and conserves surgical time. This technique exhibits excellent prosthesis-wrapping characteristics and can lead to high levels of breast satisfaction. As this study was not a prospective investigation, it limits the ability to scientifically compare surgical time, incision infections, and skin necrosis. Further validation of subsequent conclusions is warranted.
Disclosures
The authors have no conflicts of interest to declare in relation to the content of this article.
Acknowledgements
This work was supported by the Ningxia Natural Science Foundation (2024AAC03619, 2020AAC03385) and Ningxia Medical University scientific research funding special talent start-up project (XT2023039).
Materials
| Name | Company | Catalog Number | Comments |
| 10 mm Trocar with Valve | Zhejiang Tiansong Medical Instrument Co., Ltd. | TS-TK-105 | |
| 30° Laparoscopic Telescope | Karl Storz GmbH & Co. KG | 26003BA | |
| 5 mm Trocar with Valve | Zhejiang Tiansong Medical Instrument Co., Ltd. | TS-TK-105 | |
| Absorbable Suture (Vicryl 3-0) | Ethicon Endo-Surgery, Inc. | VCP375 | |
| Closed Wound Negative Pressure Drainage Set | Shandong Weigao Xinsheng Medical Instrument Co., Ltd. | PVA-20×15×1 | |
| Disposable High-Frequency Electrosurgical Pen (Hook Type, Laparoscopic-Specific) | Wuhan Banbiantian Medical Technology Development Co., Ltd. | BBT-DGB-03-23 | |
| Disposable Laparoscopic Aspirator | Wuhan Donghu Medical Technology Co., Ltd. | DH-LA-01-5×30 | |
| Disposable Open Surgery Electrosurgical Pen | Tyco Healthcare Group LP | FORCE-EZ Open | |
| Gel Breast Implant | MENTOR Worldwide LLC | SILTEX 354 | |
| Harmonic Focus (Long) Shears + Adaptive Tissue | Ethicon Endo-Surgery, Inc. | HARH36 | |
| Incision Protective Sleeve | Hubei Bokang Medical Technology Co., Ltd. | BKQYK-II | |
| SPSS | IBM | Version 25 | |
| Titanized Mesh Implant | pfm medical titanium gmbh | TiLOOP Bra | |
| V-Loc 180 Absorbable Suture (3-0) | Ethicon Endo-Surgery, Inc. | 1803H |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved