Method Article
Novel Triple-Loop Technique for Suturing TFCC Injuries without Transosseous Tunnel
In This Article
Summary
The protocol presented here introduces a new surgical technique for the treatment of triangular fibrocartilage complex injuries.
Abstract
Injuries to the triangular fibrocartilage complex (TFCC) are the most common cause of ulnar-sided wrist pain. As deepening of the research on the function and role of the TFCC, various treatment methods have emerged. Surgical treatment is often required for TFCC injuries that do not respond to conservative therapy. Currently, suturing techniques for TFCC injuries primarily include intra-capsular and transosseous tunnel suture techniques. However, traditional intra-capsular suturing has limited effectiveness for deep tears with a foveal footprint contact, while transosseous tunnel techniques pose problems such as difficulty in locating tunnels and ulna fracture. We have developed an improved triple-loop technique for treating Palmer IB-type TFCC injuries. This technique allows for suturing of both the deep and superficial layers of the TFCC without the need for a transosseous tunnel. Clinical follow-up results show that this is a safe, effective, and simple surgical method for treating TFCC injuries. In this article, we also discussed the comparison between the triple-loop surgical approach and other commonly used surgical approaches.
Introduction
TFCC is a group of important stability structures (such as articular disc, meniscal homolog, the volar and dorsal distal radioulnar ligaments, the deep layer of the ulnar extensor tendon sheath, the ulnar side of the joint capsule, the ulnar lunar ligament, and the ulnar triangular ligament) on the ulnar side of the wrist joint, including the articular disc, meniscal homolog, the volar and dorsal distal radioulnar ligaments, the deep layer of the ulnar extensor tendon sheath, the ulnar side of the joint capsule, the ulnar lunar ligament, and the ulnar triangular ligament. The volar and dorsal distal radioulnar ligaments consist of superficial and deep fibers, which converge at the attachment site on the radius. The superficial part encircles the articular disc and terminates at the ulnar styloid process, but it does not have a clearly defined insertion point. The deep part's volar and dorsal fibers converge and interlace near the insertion point to form a combined tendon, which terminates in the concave area at the base of the ulnar styloid process, which is also the ulnar attachment point of the ulnar head ligament1,2,3.
The function of the TFCC is to maintain the stability of the Distal Radioulnar Joint (DRUJ), serving as the most important structure in this region. The functions of the TFCC can be summarized in the following four points: It extends laterally from the distal radial articular surface, covering the ulnar head, thus protecting the ulnar head from direct impact. The TFCC conducts axial stress between the ulnar wrist joint and absorbs part of the load, reducing direct pressure on the joint. It forms a firm elastic connection between the distal radius and ulna, providing rotational stability. The TFCC provides support to the ulnar side of the wrist joint. Due to the complex anatomy and multiple functions of the TFCC, it is prone to injury and degeneration4,5,6.
Common causes of TFCC injuries include falling and using the hand to brace against the floor, twisting injuries from lifting heavy objects, improper use of dumbbells, and sudden forceful twisting of the wrist. The main clinical manifestations of TFCC injuries are pain on the ulnar side of the wrist joint and weakness in the wrist. This type of injury is more prevalent among physical laborers, fitness enthusiasts, young and middle-aged individuals, and thinner women7. The diagnosis of TFCC requires a combination of typical symptoms of wrist pain and weakness, as well as X-ray and MRI examinations. The preferred treatment for TFCC is conservative, with options for immobilization extending beyond or not beyond the elbow joint. The method of immobilization extending beyond the elbow joint has a higher proportion of good outcomes (76% versus 29%). For patients who do not respond to conservative treatment and whose symptoms persist for more than 3 months, surgical treatment may be considered7,8,9.
Due to the complex structure of the TFCC and varying understandings among surgeons regarding the repair of the TFCC structure, there are many different surgical methods for treating TFCC injuries9. In this article, we propose a new surgical technique called the Triple-Loop Technique. The overall goal of this technology is to improve the surgical results of TFCC injuries. The principle of developing this technology is based on a deep understanding of the anatomical structure of the TFCC. The preliminary follow-up results of this study have found that this surgical method is effective in treating TFCC injuries and has a shorter surgery duration.
Protocol
This study protocol followed the guidelines of the Human Research Ethics Committee of Shaoxing People's Hospital. Ethics approval number: 2024Z057. Informed consent was obtained from all patients included in this study. All patients agreed to use their data. Figure 1 illustrates the key steps of this surgical technique.
1. Patient selection
- Include patients with ulnar wrist pain, positive Ballotment test (instability of the distal radioulnar joint; stability rating of 2-3), ineffective and persistent symptoms after at least 2 months of conservative treatment (bracing, oral and topical medications), and MRI confirmation of the presence of TFCC injury.
- Use the following exclusion criteria: Positive variation of the ulna; a combination of the radial, distal ulna, or carpal fractures; gout, distal radioulnar arthritis, or wrist ulnar arthritis; non-type IB TFCC injury; unable to cooperate with functional rehabilitation training or unable to follow up.
- Perform the following evaluation for the patient's Visual Analogue Scale (VAS), Patient Rated Wrist Evaluation (PRWE), Disabilities of the Arm, Shoulder and Hand (DASH), grip strength, flexion, extension, rotation, etc.
2. Operative procedure
- Place the patient in the supine position and administer general anesthesia. Position the affected limb on the operating table beside the bed.
- Apply a tourniquet to the proximal upper arm. Place the tourniquet flat on the selected site, avoiding folds or twists. Secure the tourniquet with a sterile dressing, ensuring that it is stable and does not shift. Set the tourniquet pressure to 35 kPa.
- Perform Ballotment tests in the neutral position, pronation position, and supination position under anesthesia. Fix the wrist joint, pinch the ulna, and move it. If the amplitude is less than 5 mm, it is stable, and if it is greater than 5 mm, it is loose. Compare the results with those of the healthy side.
- Disinfect the affected limb with complex iodine and cover it with a waterproof surgical sheet. Abduct the shoulder joint 90° and flex the elbow joint 90°. Fix the affected limb on the traction support.
- Tuck and vertically pull the index, middle, and ring fingers. Apply a traction force of approximately 5 kg according to the graduation of the traction frame. The main unit of the arthroscopy has a 2.7 mm 30° lens. The hand-controlled mini handle used as the planer is equipped with a 2.0 mm planer head.
- Use a sterile marker to mark the 3/4, 6R, and 6U approaches. Inflate the tourniquet. Insert a 2.7 mm lens through the 3/4 approach as an observation approach. The 3/4 approach is proximal to Lister's node. If necessary, insert a needle through the 6U approach as a drainage channel. Explore the wrist joint structures radially and ulnarly, moving from proximal to distal.
NOTE: The channel of wrist arthroscopy is set based on the location of blood vessels, nerves, and tendons. For related knowledge, please refer to the research of Antonoglou et al.10. - Use the 6U and 6R approaches as the operation approach, and use a probe to explore the radial edge, central part, and ulnar edge of the TFCC microdisk. Perform a trampoline test to test the TFCC tension by pressing the fiber disc with a probe hook under the microscope to feel whether there is a trampoline-like feeling; the probe test checks the tear at the TFCC recess.
- For combined radial edge tear or central perforation tear, use a planer to clean it and use plasma shrinkage. For those with a positive probe test, use the three-loop method to suture the TFCC and use a planer to freshen the ulnar edge and recess.
- Make a 5 mm incision with a sharp knife at 1.5 cm proximal to the midpoint of the 6R and 6U approaches and use a 5 mL syringe needle to penetrate the 3-0 Polydioxanone suture (PDS) close to the anterior ulna in the posterior and superior direction, and penetrate about 2-3 mm from the ulnar edge of the TFCC. Leave the 3-0 PDS and remove the needle.
- Use the 4-0 PDS along the same approach and penetrate about 2 mm in front or behind the 3-0 PDS. Leave the 4-0 PDS and remove the needle. For the 6R approach, use mosquito forceps to pull the 3-0 and 4-0 PDS out of the same soft tissue tunnel, tie a knot with the 4-0 PDS, insert the 3-0 PDS, and use the 4-0 PDS to bring the 3-0 PDS out to complete the first loop, do not tie a knot first, and fix the end of the line with a mosquito forceps.
- Use the 6R and 6U approach, 1.5 cm proximally to the midpoint. Make an incision at 0.5 cm by a scalpel, use a 5 mL syringe needle to penetrate the 3-0 PDS close to the posterior ulna and, in an anterior-superior direction, penetrate about 2-3 mm from the ulnar edge of the TFCC. Leave the 3-0 PDS and pull out the needle.
- Use the 4-0 PDS along the same approach and penetrate about 2 mm in front or behind the 3-0 PDS. Leave the 4-0 PDS and pull out the needle. Use mosquito forceps to pull the 3-0 and 4-0 PDS out of the same soft tissue tunnel through the 6R approach, tie a knot with the 4-0 PDS, insert the 3-0 PDS, use the 4-0 PDS to bring the 3-0 PDS out, complete the second loop, do not tie a knot and use mosquito forceps to fix the end of the line and mark it.
- Through the 6U approach, insert the 3-0 PDS with a 5 mL syringe needle. Suture the TFCC from the outside to the inside, leave the 3-0 PDS, and remove the needle. Use the 4-0 PDS to directly penetrate the joint cavity through the 6U approach and use mosquito forceps to pull out the 3-0 and 4-0 PDS in the same soft tissue tunnel through the 6R approach.
- Tie a knot with the 4-0 PDS, insert the 3-0 PDS, and use the 4-0 PDS to bring the 3-0 PDS out, and complete the third loop without tying a knot. Relax the traction force and test the tension of the TFCC through the trampoline test after the three loops are tightened. When satisfied, tie knots under the skin in the order of the 1st to 3rd loops.
- After completion, perform the Ballotment test again and do the trampoline test in parallel. At this time, do not perform the hook test. Suture the incisions using 4-0 PDP sutures one by one and be careful not to suture too deep to avoid suturing the nerves and tendons.
- Apply elbow-over-elbow long-arm plaster with the elbow bent at 90° and fix it in a neutral position.
3. Postoperative rehabilitation
- Keep the elbow-over-elbow long-arm plaster for 4 weeks, during which forearm rotation, wrist flexion, and extension activities are restricted.
- Start early intervention by rehabilitation therapists after surgery, mainly to guide finger joint activities and shoulder joint activities.
- Discharge the patient from the hospital on the 1st or 2nd day after surgery. After 4 weeks, change the plaster to a broken arm brace and start activity training. After 9 weeks of surgery, the forearm and complete pronation and supination. After 6 months of surgery, the patients can participate in confrontational sports activities.
4. Efficacy evaluation
- At 1 month after surgery, re-evaluate the patient's VAS, PRWE, DASH, grip strength, flexion and extension, rotation, and other recovery conditions.
Results
We recorded the data of 20 patients who underwent the surgical method described here to treat TFCC injuries. The follow-up time of the patients ranged from 1 month to 7 months. In general, the patients had significant functional improvement after surgery. In terms of VAS score, the VAS score of the patients before surgery was 3.6 ± 0.50, and the VAS score of the patients after surgery was 1.65 ± 0.75, p < 0.0001 (Figure 2). According to another pain assessment scale, the PRWE score significantly decreased from 25.03 ± 1.82 preoperatively to 16.48 ± 6.53 postoperatively (p < 0.0001). (Figure 3). This result shows that the pain of the patients after surgery was significantly improved. DASH stands for the upper limb dysfunction score; the preoperative score was 45.42 ± 4.76, and the postoperative score was 25.66 ± 13.67, p < 0.0001 (Figure 4). The results of the grip strength test showed significant pain reduction preoperative (22.75 ± 5.79) versus postoperative (28.65 ± 6.70), p < 0.01 (Figure 5). Flexion and extension, and rotation were also significantly improved (Figure 6 and Figure 7). The above results show that this surgical method can well improve the wrist function of patients with TFCC injury. Compared with the surgical time of the bone tunnel repair of TFCC injury performed earlier, the surgical time of the triple-loop technique surgical method was significantly shorter than that of the bone tunnel surgery (25.85 ± 4.64 versus 99.00 ± 12.45, p < 0.0001; Figure 8).

Figure 1: Anatomy of the TFCC in normal and injured states and key surgical steps of the Triple-Loop Technique. The upper left corner shows the structure of the TFCC when it is normal and its appearance under MRI. The upper right corner shows the structure of the TFCC when it is damaged and its appearance under MRI. The lower left corner shows the way to pass the PDS suture through the TFCC damage during surgery. The picture in the lower right corner shows the state of the TFCC after repair. Please click here to view a larger version of this figure.

Figure 2: VAS score data. The VAS score of the patients before surgery was 3.6 ± 0.50, and the VAS score of the patients after surgery was 1.65 ± 0.75, ****p < 0.0001. The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.
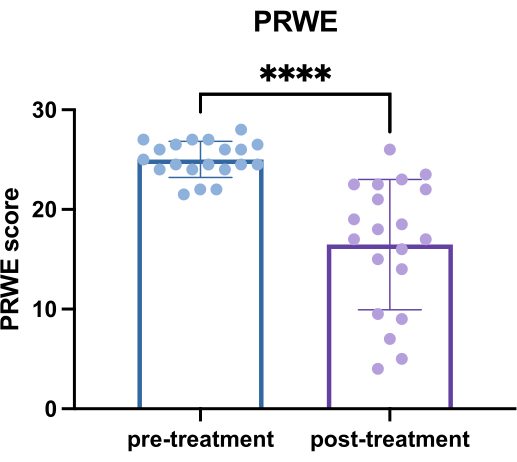
Figure 3: PRWE data. PRWE before surgery (25.03 ± 1.82) versus after surgery (16.48 ± 6.53), ****p < 0.0001. The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.

Figure 4: DASH data. DASH stands for the upper limb dysfunction score; the preoperative score was 45.42 ± 4.76, and the postoperative score was 25.66 ± 13.67, ****p < 0.0001. The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.

Figure 5: Grip Strength data. The results of the grip strength test were preoperative (22.75 ± 5.79) versus postoperative (28.65 ± 6.70), **p < 0.01. The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.

Figure 6: Flexion data. The results of the flexion were preoperative (129.00 ± 4.472) versus postoperative (154.50 ± 5.59), ****p < 0.0001. The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.

Figure 7: Rotation data. The results of the rotation were preoperative (135.00 ± 7.07) versus postoperative (159.80 ± 9.10), ****p < 0.01. The error bars show standard error. The t test was used for comparison among groups. The y-axis represents the angle in °. Please click here to view a larger version of this figure.

Figure 8: Surgery duration. The surgical time of the Triple-Loop Technique surgical method was significantly shorter than that of the bone tunnel surgery (25.85 ± 4.64 versus 99.00 ± 12.45, p < 0.0001). The error bars show standard error. The t test was used for comparison among groups. Please click here to view a larger version of this figure.
Discussion
The classic classification of TFCC is based on Plamer et al. proposed in 198911. According to the location of the injury, TFCC injuries are divided into four types: IA, IB, IC, and ID. Type IA is a traumatic central tear, and type IB is a traumatic ulnar-sided tear, sometimes with concomitant avulsion of the styloid process. Type IC is a traumatic peripheral tear incorporating the ulnolunate and ulnotriquetral ligaments. Type ID is a traumatic radial-sided tear, sometimes with concomitant fracture of the sigmoid notch11. However, Plamer's classification does not pay enough attention to the hammock concept of TFCC structure, ulnar foveal, and deep branch. In response to the above defects, one study further classified the Plamer 1-B type in 200912. It divided the types into distal tears, complete tears, proximal tears, and complete tears combined with interosseous membrane injury. Among these types, distal tears account for about 27%, and complete tears and proximal tears account for more than 70%13. This means that more than 70% of TFCC injuries are foveal tears. This type of injury requires repair of both the superficial branch of the TFCC and the deep branch13.
Before 2008, the treatment of foveal tears was basically open surgery. With the development of arthroscopic technology and researchers' further understanding of the TFCC structure, after 2008, the treatment of TFCC was basically arthroscopic surgery14.
There are many options for arthroscopic surgery of TFCC, such as different ways of joint capsule suturing, rivets, or bone tunnel repair14. One study introduced15 a fully arthroscopic technique that uses rivets to repair TFCC foveal tears. This technique can significantly improve patients' pain, stability, and function. Most patients resume normal work and sports activities after surgery with fewer complications. This technique can better repair TFCC injuries, but it requires the use of additional consumables.
One study16 summarized a method of repairing TFCC by establishing a bone tunnel on the ulna, creating a small 1.6 mm bone tunnel on the radial edge of the fovea, and inserting four sutures into the tunnel using a 16G needle. These four sutures can be used to suture the TFCC under arthroscopy and press it against the fovea. It provides a good suture structure for the reattachment of the TFCC fovea and also provides an anatomical contact surface for the healing between the torn TFCC and its foveal footprint16. This technique does not require the use of additional rivets, and repairing TFCC through a bone tunnel is a good surgical method17,18. However, bone tunnel surgery is difficult to operate. It requires a high level of proficiency. In addition, the ulnar styloid process is small, and complications such as fractures are prone to occur during the operation. Compared with this method of fixing TFCC through a bone tunnel, the surgical method we mentioned in this article has the advantages of shorter operation time and simpler operation.
Another study proposed a method of joint capsule suturing, making two incisions at the proximal end of 6R and 6U and repairing TFCC with a 3-0 polydioxanone horizontal mattress suture. These two sutures function like horse bridles, fixing the TFCC on the concave footprint of the cartilage complex19. Based on the creativity brought by this surgical method, we proposed the surgical method introduced in this article. In the described surgical method, the main focus is on the ulnar deep branch of the TFCC. However, this method provides a very convenient way to repair the ulnar deep branch without the need for bone tunnels and rivets. It has the advantages of convenience and a good economy. However, this surgical method ignores the ulnar superficial branch of the TFCC. Based on this, we propose improvements to the earlier surgical method. In this modified surgical method, we repaired the ulnar superficial branch and deep branch at the same time. At the same time, the operation only used one skin incision to repair the ulnar deep branch of the TFCC. Because this surgical method can see two loops of the deep branch and one loop of the superficial branch under arthroscopy, we named this surgical method the Triple-Loop Technique.
In general, this article introduces a new surgical method for repairing TFCC injuries, which has the advantages of convenience, economy, simple operation, and fewer skin incisions. The specific steps are described in step 1.3 and Figure 1. In summary, the deep and superficial branches of TFCC are repaired simultaneously with sutures in a minimally invasive manner, without the need for anchors or bone tunnels. However, this technology has a shortcoming: it must be performed under arthroscopy. This cannot be done in some hospitals that lack arthroscopic equipment. The invention of this technology is an innovation of the existing TFCC repair surgery. It also reminds doctors to pay more attention to the deep branch of TFCC.
Disclosures
All authors declare there is no conflict in this study.
Acknowledgements
This study is supported by the Shaoxing Health Science and Technology Plan Project (2023SKY013) and the Zhejiang Provincial Medical and Health Planning Project (2020KY979).
Materials
| Name | Company | Catalog Number | Comments |
| Arthroscopic machine | Smith and Nephew | 4K | Arthroscopic imaging system |
| Automatic Tourniquet System | ULAND | ATSB-III | Reduce surgical bleeding |
| complex iodine | annjet | annjet-001 | Skin disinfection |
| Planer handle | Smith and Nephew | 72201500 | Synovial cleaning and wound freshening |
| Polydioxanone suture | Johnson and Johnson | PDP774D | Sutures |
| Wrist joint traction system | Smith and Nephew | 72202114 | Surgical traction |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved