Peripheral Vascular Exam Using a Continuous Wave Doppler
Overview
Source: Joseph Donroe, MD, Internal Medicine and Pediatrics, Yale School of Medicine, New Haven, CT
Peripheral vascular disease (PVD) is a common condition affecting older adults and includes disease of the peripheral arteries and veins. While the history and physical exam offer clues to its diagnosis, Doppler ultrasound has become a routine part of the bedside vascular examination. The video titled "The Peripheral Vascular Exam" gave a detailed review of the physical examination of the peripheral arterial and venous systems. This video specifically reviews the bedside assessment of peripheral arterial disease (PAD) and chronic venous insufficiency using a handheld continuous wave Doppler.
The handheld Doppler (HHD) is a simple instrument that utilizes continuous transmission and reception of ultrasound (also referred to as continuous wave Doppler) to detect changes in blood velocity as it courses through a vessel. The Doppler probe contains a transmitting element that emits ultrasound and a receiving element that detects ultrasound waves (Figure 1). The emitted ultrasound is reflected off of moving blood and back to the probe at a frequency directly related to the velocity of blood flow. The reflected signal is detected and transduced to an audible sound with a frequency directly related to that of the received Doppler signal (thus, faster blood flow produces a higher frequency sound).
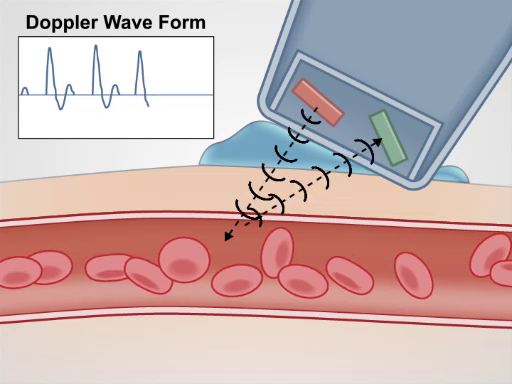
Figure 1. Generation of a Doppler signal. The handheld Doppler emits an ultrasound signal, which is then reflected back by moving blood, and finally received by the Doppler probe.
The HHD is easily used in the office or hospital setting to detect pulses, screen for PAD using the ankle brachial pressure index (ABPI), and localize venous insufficiency. This video reviews these procedures; however, it is not intended to be a comprehensive review of non-invasive vascular testing.
Procedure
1. Preparation
- Obtain a blood pressure cuff, an HHD machine, Doppler gel, and skin marker.
- Wash hands prior to examining the patient.
- Begin with the patient in a gown, lying comfortably supine on the exam table.

Figure 2. The major arteries of the upper and lower extremities.
2. Lower Extremity Arterial Assessment
- For patients with weak or absent pulses by palpation, or historical risk factors for peripheral arterial disease (PAD), use the HHD to assess blood flow. Begin by applying gel in the expected area of the artery being investigated ( Figure 2).
- Place the Doppler over the artery at a 45 degree angle to the skin, pointing cephalad. If the Doppler signal is not detected, slowly move the Doppler probe medially and laterally, as occasionally, the path of distal arteries can vary. Remember that a small percentage of people may have a congenitally absent dorsalis pedal (DP) artery.
- If a signal is encountered, note the character of the sound wave produced. While some HHD have a screen or can print out the waveform to view, the shape can also be determined by listening. A normal arterial waveform in the lower extremity is triphasic (Figure 3). The first component of the wave occurs in systole and is generated by the rapid flow of blood toward the probe, generating a high frequency wave. At the end of systole and beginning of diastole, blood flow slows and reverses direction, resulting in a second, lower frequency wave. Finally, forward returns at the end of diastole, producing the low frequency third wave. Distal to an arterial stenosis, the amplitude of the waveform becomes progressively dampened with loss of flow reversal, resulting in a monophasic waveform. Immediately over a partially stenosed segment of artery, the flow velocity is increased, producing a high frequency wave. Complete arterial occlusion without collateral flow leads to absence of flow distally and no signal generation.
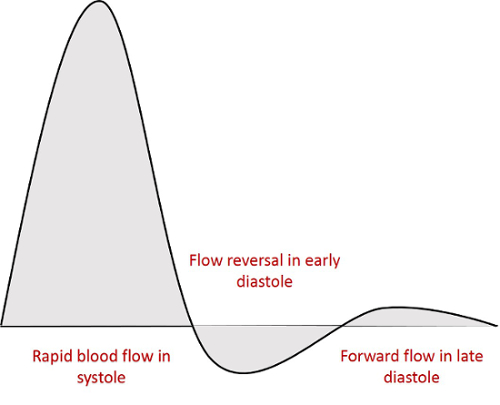
Figure 3. The triphasic Doppler arterial waveform. The initial large deflection is forward blood flow during systole. The second deflection is the reversal of flow in early diastole. The third deflection is return of forward flow in late diastole.
- If frequent reassessment is necessary, mark the location where the arterial pulse is found.
- If there is suspicion for peripheral arterial disease based on the history or physical exam, calculate the ankle brachial pulse index (ABPI). Prior to performing the procedure, have the patient lie supine and relax for 10 min, with both the upper and lower extremities at the level of the heart.
- Place the appropriately-sized blood pressure (BP) cuff on the upper arm. Make sure the cuff bladder length is at least 80% and the bladder width at least 40% of the arm circumference.
- Apply gel to the antecubital fossa medial to the biceps tendon and find the brachial artery with the HHD.
- Inflate the cuff until the Doppler signal disappears.
- Slowly deflate the cuff. The first Doppler signal heard reflects the systolic pressure. Record this number and repeat the process in the other arm.
- Place the appropriately sized BP cuff on the lower extremity, just proximal to the ankle.
- Apply gel to the dorsum of the foot lateral to the extensor hallucis longus tendon and use the HHD to find the DP artery.
- Inflate the cuff until the Doppler signal disappears.
- Slowly deflate the cuff. The first Doppler signal heard reflects the systolic pressure. Record this number and repeat the process over the posterior tibialis (PT) artery.
- Repeat this on the other leg.
- Calculate the ABPI for a given leg by dividing the higher systolic pressure of the DP or PT artery in that leg with the higher of the two brachial artery systolic pressures. Table 1 shows the interpretation of the ABPI.
| ABPI of leg A = Higher pedal pressure of leg A / Higher brachial pressure (A or B) | |
| Value | Interpretation |
| >1.4 | Non-compressible, calcified arteries |
| 1.0-1.4 | Normal range |
| 0.91-0.99 | Borderline |
| 0.41-0.90 | Mild to moderate peripheral arterial disease |
| <0.4 | Severe peripheral arterial disease |
Table 1: Interpretation of the Ankle Brachial Pressure Index (ABPI).
- Assess for venous insufficiency of the lower extremity in patients with edema or varicose veins. Have the patient in the standing position with their weight shifted onto the unexamined leg.
- Apply a generous amount of gel and place the HHD over the femoral artery, just below the inguinal ligament. Slowly move the probe medially, while squeezing and releasing the ipsilateral calf muscle to generate audible flow through the venous system. Once the HHD transmits this signal clearly, it is in the vicinity of the saphenofemoral junction (SFJ).
- Move just inferior and medial to the SFJ to isolate the distal segment of the greater saphenous vein (GSV).
- Squeeze the calf muscle and listen for normal augmentation of flow.
- Release the calf muscle. Re-augmentation of flow lasting more than 1 sec is abnormal and represents retrograde flow through an incompetent valve at the SFJ.
- Move to the medial thigh, approximately 10 cm above the knee along the expected path of the GSV, and apply gel.
- Place the probe on the skin, while squeezing the calf muscle. The probe is well positioned once a clear signal is heard.
- Squeeze the calf muscle and listen for normal augmentation of flow.
- Release the calf muscle. Re-augmentation of flow lasting more than 1 sec may be heard with SFJ reflux, incompetent thigh perforator veins, or incompetent valves within the GSV proximal to the HHD probe.
- Move behind the patient and place gel in the popliteal fossa.
- Use the probe to find the popliteal artery, then move medially, while squeezing the calf muscle, to find the popliteal vein.
- Once well-positioned over the popliteal vein, squeeze the calf muscle and listen for normal augmentation of flow.
- Release the calf muscle. The venous anatomy around the popliteal fossa is complex, and re-augmentation of flow lasting more than 1 sec usually cannot be localized to one particular superficial or deep vein. Rather, it may represent reflux at the saphenopopliteal junction (SPJ), the small saphenous vein, tributaries of the GSV, or calf veins.
Application and Summary
A careful history and physical exam are important for anyone suspected of peripheral vascular disease based on symptoms or risk factors. The HHD has become part of the routine bedside vascular examination and should be used to complement the physical exam, if PVD is suspected. It is not a technically difficult tool to use, and the maneuvers described in the video can be performed by general physicians. Just like for the physical exam, knowledge of the vascular anatomy is critical to the success of the HHD exam.
Vascular assessment by HHD has some important limitations. A false positive Doppler signal may occur over an artery distal to a total occlusion, if sufficient collateral flow has developed, leading to the inaccurate belief that PAD is not present. Additionally, the ABI may be falsely high in calcified vessels as they become less compressible. This is particularly relevant to diabetic patients. Venous testing by HHD is far more accurate for localizing valvular reflux than physical exam maneuvers, such as the Brodie-Trendelenburg test, cough test, and Perthes test; however, it is still less accurate than color duplex scanning. Finally, while there is some literature describing HHD testing for deep vein thrombosis, this is not considered standard of care, and thus, it is not reviewed here. If clinical suspicion for peripheral vascular disease persists despite reassuring physical exam and HHD testing, more formal vascular testing should be performed by a vascular specialist.
Skip to...
Videos from this collection:

Now Playing
Peripheral Vascular Exam Using a Continuous Wave Doppler
Physical Examinations I
38.5K Views

General Approach to the Physical Exam
Physical Examinations I
116.0K Views

Observation and Inspection
Physical Examinations I
93.3K Views

Palpation
Physical Examinations I
82.9K Views

Percussion
Physical Examinations I
99.9K Views

Auscultation
Physical Examinations I
60.5K Views

Proper Adjustment of Patient Attire during the Physical Exam
Physical Examinations I
83.2K Views

Blood Pressure Measurement
Physical Examinations I
107.5K Views

Measuring Vital Signs
Physical Examinations I
114.1K Views

Respiratory Exam I: Inspection and Palpation
Physical Examinations I
156.9K Views

Respiratory Exam II: Percussion and Auscultation
Physical Examinations I
212.4K Views

Cardiac Exam I: Inspection and Palpation
Physical Examinations I
176.0K Views

Cardiac Exam II: Auscultation
Physical Examinations I
139.5K Views

Cardiac Exam III: Abnormal Heart Sounds
Physical Examinations I
91.6K Views

Peripheral Vascular Exam
Physical Examinations I
68.1K Views
Copyright © 2025 MyJoVE Corporation. All rights reserved